Monday Poster Session
Category: GI Bleeding
P2532 - Trust Your Gut: A Case of Methamphetamine-Induced Gastrointestinal Ischemia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NJ
Nicole Johnsen, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Nicole Johnsen, BS1, Andrew Chang, MD1, Kelley Chuang, MD2, Satya Patel, MD2, Simon Wu, MD2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Methamphetamine is widely used with extensively reported cardiovascular and cerebrovascular complications, but its gastrointestinal effects are less known. Although rare, methamphetamine-induced gastrointestinal ischemia has high morbidity and mortality, with limited case reports.
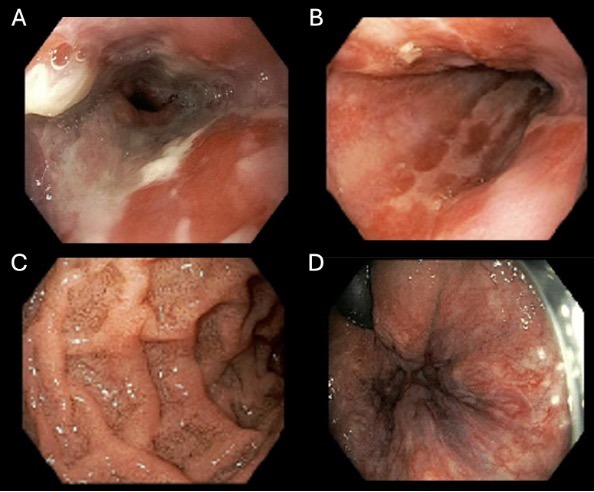
Case Description/Methods: We present a case of a 48-year-old man with two weeks of episodic abdominal pain. He developed acute, severe abdominal pain after a large meal, accompanied by nausea and hematemesis. He also noted twenty pounds of unintentional weight loss over one year. His medical history was significant for gastroesophageal reflux disease, alcohol use disorder in remission, and previously charted inhaled and intranasal methamphetamine use. Notably, he had not taken his omeprazole for the past year. Laboratory studies were notable for a hemoglobin drop from 15.5 g/dL on admission to 13.4 g/dL two days later. Computed tomography of the abdomen and pelvis showed wall thickening of the distal esophagus and distal stomach, and luminal narrowing in the mid transverse colon. Although the patient denied recent intentional methamphetamine use, urine toxicology and confirmatory testing were positive for amphetamines. Esophagogastroduodenoscopy (EGD) and colonoscopy revealed diffuse ulcerations in the distal esophagus and post-pyloric region, and pale mucosa in the stomach and colon most pronounced at the splenic flexure with no masses or strictures. EGD pathology showed active and chronic inflammation in the distal esophagus, stomach and post-pylorus regions, as well as metaplasia, but no dysplasia or malignancy. Immunohistochemical staining for H. pylori was positive from the gastroesophageal junction but negative from an antral ulcer. No colonic biopsies were taken. Though his H. pylori infection could explain some of his findings, his history of methamphetamine use, and diffuse endoscopic and pathology findings were also highly suggestive of methamphetamine-induced ischemia. He was counseled to avoid stimulants, prescribed quadruple therapy for H. pylori, and discharged with a plan for repeat EGD in two months.
Discussion: This case emphasizes the importance of taking a thorough social history. We highlight the importance of considering amphetamine-induced gastrointestinal ischemia in patients with previously documented substance use disorder presenting with acute abdominal pain. Early recognition of this etiology can lead to more targeted counseling and improved outcomes.
Disclosures:
Nicole Johnsen, BS1, Andrew Chang, MD1, Kelley Chuang, MD2, Satya Patel, MD2, Simon Wu, MD2. P2532 - Trust Your Gut: A Case of Methamphetamine-Induced Gastrointestinal Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Methamphetamine is widely used with extensively reported cardiovascular and cerebrovascular complications, but its gastrointestinal effects are less known. Although rare, methamphetamine-induced gastrointestinal ischemia has high morbidity and mortality, with limited case reports.
Case Description/Methods: We present a case of a 48-year-old man with two weeks of episodic abdominal pain. He developed acute, severe abdominal pain after a large meal, accompanied by nausea and hematemesis. He also noted twenty pounds of unintentional weight loss over one year. His medical history was significant for gastroesophageal reflux disease, alcohol use disorder in remission, and previously charted inhaled and intranasal methamphetamine use. Notably, he had not taken his omeprazole for the past year. Laboratory studies were notable for a hemoglobin drop from 15.5 g/dL on admission to 13.4 g/dL two days later. Computed tomography of the abdomen and pelvis showed wall thickening of the distal esophagus and distal stomach, and luminal narrowing in the mid transverse colon. Although the patient denied recent intentional methamphetamine use, urine toxicology and confirmatory testing were positive for amphetamines. Esophagogastroduodenoscopy (EGD) and colonoscopy revealed diffuse ulcerations in the distal esophagus and post-pyloric region, and pale mucosa in the stomach and colon most pronounced at the splenic flexure with no masses or strictures. EGD pathology showed active and chronic inflammation in the distal esophagus, stomach and post-pylorus regions, as well as metaplasia, but no dysplasia or malignancy. Immunohistochemical staining for H. pylori was positive from the gastroesophageal junction but negative from an antral ulcer. No colonic biopsies were taken. Though his H. pylori infection could explain some of his findings, his history of methamphetamine use, and diffuse endoscopic and pathology findings were also highly suggestive of methamphetamine-induced ischemia. He was counseled to avoid stimulants, prescribed quadruple therapy for H. pylori, and discharged with a plan for repeat EGD in two months.
Discussion: This case emphasizes the importance of taking a thorough social history. We highlight the importance of considering amphetamine-induced gastrointestinal ischemia in patients with previously documented substance use disorder presenting with acute abdominal pain. Early recognition of this etiology can lead to more targeted counseling and improved outcomes.
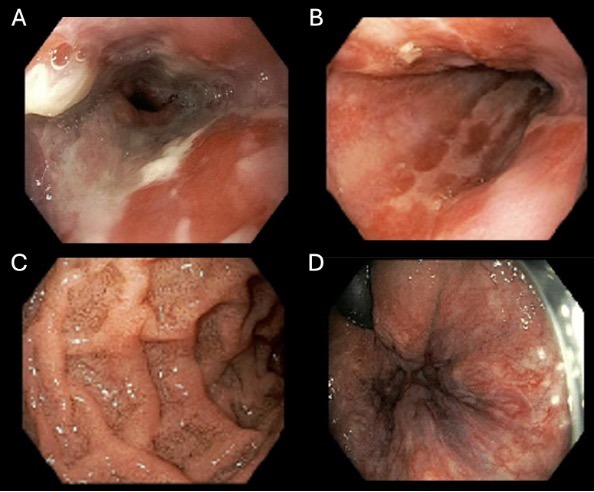
Figure: Endoscopy revealed ulcerations in the distal esophagus (Fig 1A) and post-pyloric region (Fig 1B), as well as pale mucosa in the stomach (Fig 1C) and colon most pronounced at the splenic flexure (Fig 1D).
Disclosures:
Nicole Johnsen indicated no relevant financial relationships.
Andrew Chang indicated no relevant financial relationships.
Kelley Chuang indicated no relevant financial relationships.
Satya Patel indicated no relevant financial relationships.
Simon Wu: Glass Health – Independent Contractor.
Nicole Johnsen, BS1, Andrew Chang, MD1, Kelley Chuang, MD2, Satya Patel, MD2, Simon Wu, MD2. P2532 - Trust Your Gut: A Case of Methamphetamine-Induced Gastrointestinal Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
