Monday Poster Session
Category: GI Bleeding
P2444 - Impact of Ostomy on Clinical Outcomes in Patients Hospitalized With Gastrointestinal Bleeding: A Retrospective Cohort Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Adejoke Johnson, MD
Jacobi Medical Center/North Central Bronx Hospital
Bronx, NY
Presenting Author(s)
Adejoke Johnson, MD1, Ezekiel Akpan, MD1, Marianne E. Solano, MD2, Dharshana Prem Anand, MD3, Rahul Kumar, MD4, Donald P. Kotler, MD5
1Jacobi Medical Center/North Central Bronx Hospital, Bronx, NY; 2University of Carabobo, School of Medicine, Aragua, Houston, TX; 3NYC Health + Hospitals/Jacobi, Bronx, NY; 4Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 5Jacobi Medical Center/North Central Bronx Hospital/Albert Einstein College of Medicine, Bronx, NY
Introduction: Gastrointestinal (GI) bleeding significantly complicates the management of patients with artificial openings (ostomy) of the gastrointestinal tract. This study explores the impact of ostomies on clinical outcomes among patients hospitalized with GI bleeding.
Methods: We conducted a retrospective cohort analysis using the National Inpatient Sample (NIS) data from 2016 to 2020, focusing on patients primarily diagnosed with GI bleeding as defined by the International Classification of Diseases, 10th Revision. Hospitalizations for GI bleeding were stratified based on the presence of an ostomy (such as gastrostomy, ileostomy, or colostomy). The primary endpoint was in-hospital mortality. Secondary outcomes included total and early (< 24hrs from admission) esophagogastroduodenoscopy (EGD) and colonoscopy rates, procedural interventions, and angiography and IR embolization. We used STATA software for multivariate logistic and linear regression analyses to compare outcomes, control for confounders, and identify mortality predictors.
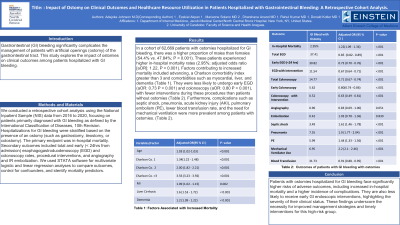
Results: In a cohort of 62,669 patients with ostomies hospitalized for GI bleeding, there was a higher proportion of males than females (54.4% vs. 47.84%; P < 0.001). These patients experienced higher in-hospital mortality rates (2.95%; adjusted odds ratio [aOR]: 1.22, P < 0.001). Factors contributing to increased mortality included advancing age (aOR: 1.03 P < 0.001), a Charlson comorbidity index greater than 3 (aOR: 3.56 P < 0.001), and comorbidities such as myocardial infarction (aOR: 1.09 P=0.002), liver cirrhosis (aOR: 1.6 P < 0.001), and dementia (aOR: 1.2 P < 0.001). They were less likely to undergo early EGD (aOR: 0.73 P < 0.001) and colonoscopy (aOR: 0.80 P < 0.001), with fewer interventions during these procedures than patients without ostomies (Table 1). Furthermore, complications such as septic shock, pneumonia, acute kidney injury (AKI), pulmonary embolism (PE), lower blood transfusion rate, and the need for mechanical ventilation were more prevalent among patients with ostomies. (Table 1).
Discussion: Patients with ostomies hospitalized for GI bleeding face significantly higher risks of adverse outcomes, including increased in-hospital mortality and a higher incidence of complications. They are also less likely to receive early GI endoscopic interventions, highlighting the severity of their clinical status. These findings underscore the necessity for improved management strategies and timely interventions for this high-risk group.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Adejoke Johnson, MD1, Ezekiel Akpan, MD1, Marianne E. Solano, MD2, Dharshana Prem Anand, MD3, Rahul Kumar, MD4, Donald P. Kotler, MD5. P2444 - Impact of Ostomy on Clinical Outcomes in Patients Hospitalized With Gastrointestinal Bleeding: A Retrospective Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jacobi Medical Center/North Central Bronx Hospital, Bronx, NY; 2University of Carabobo, School of Medicine, Aragua, Houston, TX; 3NYC Health + Hospitals/Jacobi, Bronx, NY; 4Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 5Jacobi Medical Center/North Central Bronx Hospital/Albert Einstein College of Medicine, Bronx, NY
Introduction: Gastrointestinal (GI) bleeding significantly complicates the management of patients with artificial openings (ostomy) of the gastrointestinal tract. This study explores the impact of ostomies on clinical outcomes among patients hospitalized with GI bleeding.
Methods: We conducted a retrospective cohort analysis using the National Inpatient Sample (NIS) data from 2016 to 2020, focusing on patients primarily diagnosed with GI bleeding as defined by the International Classification of Diseases, 10th Revision. Hospitalizations for GI bleeding were stratified based on the presence of an ostomy (such as gastrostomy, ileostomy, or colostomy). The primary endpoint was in-hospital mortality. Secondary outcomes included total and early (< 24hrs from admission) esophagogastroduodenoscopy (EGD) and colonoscopy rates, procedural interventions, and angiography and IR embolization. We used STATA software for multivariate logistic and linear regression analyses to compare outcomes, control for confounders, and identify mortality predictors.
Results: In a cohort of 62,669 patients with ostomies hospitalized for GI bleeding, there was a higher proportion of males than females (54.4% vs. 47.84%; P < 0.001). These patients experienced higher in-hospital mortality rates (2.95%; adjusted odds ratio [aOR]: 1.22, P < 0.001). Factors contributing to increased mortality included advancing age (aOR: 1.03 P < 0.001), a Charlson comorbidity index greater than 3 (aOR: 3.56 P < 0.001), and comorbidities such as myocardial infarction (aOR: 1.09 P=0.002), liver cirrhosis (aOR: 1.6 P < 0.001), and dementia (aOR: 1.2 P < 0.001). They were less likely to undergo early EGD (aOR: 0.73 P < 0.001) and colonoscopy (aOR: 0.80 P < 0.001), with fewer interventions during these procedures than patients without ostomies (Table 1). Furthermore, complications such as septic shock, pneumonia, acute kidney injury (AKI), pulmonary embolism (PE), lower blood transfusion rate, and the need for mechanical ventilation were more prevalent among patients with ostomies. (Table 1).
Discussion: Patients with ostomies hospitalized for GI bleeding face significantly higher risks of adverse outcomes, including increased in-hospital mortality and a higher incidence of complications. They are also less likely to receive early GI endoscopic interventions, highlighting the severity of their clinical status. These findings underscore the necessity for improved management strategies and timely interventions for this high-risk group.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Adejoke Johnson indicated no relevant financial relationships.
Ezekiel Akpan indicated no relevant financial relationships.
Marianne Solano indicated no relevant financial relationships.
Dharshana Prem Anand indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Donald P. Kotler: EMD Serono – Consultant.
Adejoke Johnson, MD1, Ezekiel Akpan, MD1, Marianne E. Solano, MD2, Dharshana Prem Anand, MD3, Rahul Kumar, MD4, Donald P. Kotler, MD5. P2444 - Impact of Ostomy on Clinical Outcomes in Patients Hospitalized With Gastrointestinal Bleeding: A Retrospective Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
