Monday Poster Session
Category: GI Bleeding
P2453 - Patient Outcomes Related to Acuity and Time to Endoscopy for Upper Gastrointestinal Bleeding: A Retrospective Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Brian Lee, DO
Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center
San Antonio, TX
Presenting Author(s)
Brian Lee, DO1, Gian Galura, MD2, Jeff Taclob, MD3, Swati Mahapatra, DO2, Shivangini Duggal, MD4, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Monica Botros, MD2, Alejandro Robles, MD3, Vishwajeet Singh, PhD2, Alok Dwivedi, PhD5, Marc Zuckerman, MD2, Sherif E.. Elhanafi, MD2
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, San Antonio, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4TTUHSC, El Paso, TX; 5Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Upper gastrointestinal bleeding (UGIB) is a common medical emergency with mortality rates ranging from 2% to 15%. The optimal timing of endoscopy is variable among current literature with conflicting reported clinical outcomes. This study aimed to assess the impact of patient acuity and the timing of endoscopic intervention on clinical outcomes.
Methods: A retrospective cohort study was performed on adults who were admitted to a tertiary care center with UGIB and underwent EGD from July 1, 2017, to July 31, 2022. Demographics, clinical characteristics, endoscopic findings, and patient outcomes were reviewed. Presenting Shock Index (SI) was utilized to stratify subjects by acuity and further categorized by timing of EGD (early ≤24 vs late >24 hours). Fisher’s exact and Wilcoxon rank-sum tests were utilized.
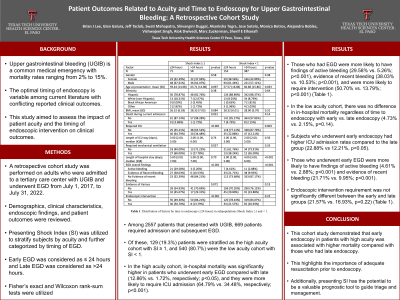
Results: Among 2557 patients that presented with UGIB, 669 patients required admission and subsequent EGD. Of these, 129 (19.3%) patients were stratified as the high acuity cohort with SI ≥1, and 540 (80.7%) were the low acuity cohort with SI < 1.
In the high acuity cohort, in-hospital mortality was significantly higher in patients who underwent early EGD compared with late (12.86% vs 1.72%; p< 0.05), and they were more likely to require ICU admission (64.79% vs 34.48%, respectively; p< 0.001). Those who had EGD were more likely to have findings of active bleeding (29.58% vs 5.26%; p< 0.001), evidence of recent bleeding (38.03% vs 10.53%; p< 0.001), and were more likely to require intervention (50.70% vs. 13.79%; p< 0.001) (Table 1).
In the low acuity cohort, there was no difference in in-hospital mortality regardless of time to endoscopy with early vs late endoscopy (4.73% vs 2.15%; p=0.14). Subjects who underwent early endoscopy had higher ICU admission rates compared to the late group (22.88% vs 12.21%, p< 0.05). Those who underwent early EGD were more likely to have findings of active bleeding (4.61% vs 2.88%; p< 0.001) and evidence of recent bleeding (21.71% vs 9.95%; p< 0.001). Endoscopic intervention requirement was not significantly different between the early and late groups (21.57% vs 16.93%, p = 0.22) (Table 1).
Discussion: This cohort study demonstrated that early endoscopy in patients with high acuity was associated with higher mortality compared with those who had late endoscopy. This highlights the importance of adequate resuscitation prior to endoscopy. Additionally, presenting SI has the potential to be a valuable prognostic tool to guide triage and management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian Lee, DO1, Gian Galura, MD2, Jeff Taclob, MD3, Swati Mahapatra, DO2, Shivangini Duggal, MD4, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Monica Botros, MD2, Alejandro Robles, MD3, Vishwajeet Singh, PhD2, Alok Dwivedi, PhD5, Marc Zuckerman, MD2, Sherif E.. Elhanafi, MD2. P2453 - Patient Outcomes Related to Acuity and Time to Endoscopy for Upper Gastrointestinal Bleeding: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, San Antonio, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4TTUHSC, El Paso, TX; 5Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Upper gastrointestinal bleeding (UGIB) is a common medical emergency with mortality rates ranging from 2% to 15%. The optimal timing of endoscopy is variable among current literature with conflicting reported clinical outcomes. This study aimed to assess the impact of patient acuity and the timing of endoscopic intervention on clinical outcomes.
Methods: A retrospective cohort study was performed on adults who were admitted to a tertiary care center with UGIB and underwent EGD from July 1, 2017, to July 31, 2022. Demographics, clinical characteristics, endoscopic findings, and patient outcomes were reviewed. Presenting Shock Index (SI) was utilized to stratify subjects by acuity and further categorized by timing of EGD (early ≤24 vs late >24 hours). Fisher’s exact and Wilcoxon rank-sum tests were utilized.
Results: Among 2557 patients that presented with UGIB, 669 patients required admission and subsequent EGD. Of these, 129 (19.3%) patients were stratified as the high acuity cohort with SI ≥1, and 540 (80.7%) were the low acuity cohort with SI < 1.
In the high acuity cohort, in-hospital mortality was significantly higher in patients who underwent early EGD compared with late (12.86% vs 1.72%; p< 0.05), and they were more likely to require ICU admission (64.79% vs 34.48%, respectively; p< 0.001). Those who had EGD were more likely to have findings of active bleeding (29.58% vs 5.26%; p< 0.001), evidence of recent bleeding (38.03% vs 10.53%; p< 0.001), and were more likely to require intervention (50.70% vs. 13.79%; p< 0.001) (Table 1).
In the low acuity cohort, there was no difference in in-hospital mortality regardless of time to endoscopy with early vs late endoscopy (4.73% vs 2.15%; p=0.14). Subjects who underwent early endoscopy had higher ICU admission rates compared to the late group (22.88% vs 12.21%, p< 0.05). Those who underwent early EGD were more likely to have findings of active bleeding (4.61% vs 2.88%; p< 0.001) and evidence of recent bleeding (21.71% vs 9.95%; p< 0.001). Endoscopic intervention requirement was not significantly different between the early and late groups (21.57% vs 16.93%, p = 0.22) (Table 1).
Discussion: This cohort study demonstrated that early endoscopy in patients with high acuity was associated with higher mortality compared with those who had late endoscopy. This highlights the importance of adequate resuscitation prior to endoscopy. Additionally, presenting SI has the potential to be a valuable prognostic tool to guide triage and management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian Lee indicated no relevant financial relationships.
Gian Galura indicated no relevant financial relationships.
Jeff Taclob indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Akanksha Togra: Clinexel Inc – Owner/Ownership Interest. Clinexel Life Sciences Pvt Ltd – Owner/Ownership Interest. Cytenet Life science LLP – Owner/Ownership Interest. GLRK Healthcare foundation (Non-profit Organization Company) – Owner/Ownership Interest.
Jose Sotelo indicated no relevant financial relationships.
Monica Botros indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Vishwajeet Singh indicated no relevant financial relationships.
Alok Dwivedi indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Brian Lee, DO1, Gian Galura, MD2, Jeff Taclob, MD3, Swati Mahapatra, DO2, Shivangini Duggal, MD4, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Monica Botros, MD2, Alejandro Robles, MD3, Vishwajeet Singh, PhD2, Alok Dwivedi, PhD5, Marc Zuckerman, MD2, Sherif E.. Elhanafi, MD2. P2453 - Patient Outcomes Related to Acuity and Time to Endoscopy for Upper Gastrointestinal Bleeding: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
