Monday Poster Session
Category: GI Bleeding
P2454 - The Efficacy of Colonoscopy and Flexible Sigmoidoscopy in Diverticular Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gurjot Singh, DO
The Warren Alpert Medical School of Brown University
Warwick, RI
Presenting Author(s)
Kailtyn M. Egger, DO1, Gurjot Singh, DO2, Cristina Hamacher, DO1, Rachel Bednarz-Medeiros, DO3, Angela Fishman, DO4
1Kent Hospital, Warwick, RI; 2The Warren Alpert Medical School of Brown University, Warwick, RI; 3Brown University / Warren Alpert Medical School, Warwick, RI; 4University Gastroenterology, East Greenwich, RI
Introduction: Diverticular bleeding affecting 0.46 patients per 1,000 patients/year caused by ulceration of either the neck or dome of a diverticula, can lead to significant arterial gastrointestinal bleeding. Management of diverticular bleeding can be complicated by the intermittent nature of this type of bleeding, making it difficult to achieve hemostasis by both angiography and colonoscopy. Multiple studies have shown that early colonoscopy does not improve outcomes compared to colonoscopy at a later. Therefore, the current American College of Gastroenterology guidelines on suspected diverticular bleeding advise that if there is continued lower GI bleeding the initial diagnostic test to be used is a CTA, if positive patients should undergo interventional radiology intervention without delay. Colonoscopy can also be considered with a positive CTA or when bleeding does not subside and the patient has not had a colonoscopy within the previous year. In this project, I examine the efficacy of colonoscopy in identifying active diverticular bleeding in those who have undergone colonoscopy or flexible sigmoidoscopy within 48 hours of presentation for ongoing lower GI bleeding.
Methods: A retrospective single-center chart review was conducted on all adult patients who underwent a colonoscopy or flexible sigmoidoscopy at Kent Hospital, Warwick, RI from January 1, 2020 - June 1, 2023. Outpatient colonoscopies and flexible sigmoidoscopies were eliminated from the review process. Elements evaluated were consult note differential diagnosis and findings on the procedure.
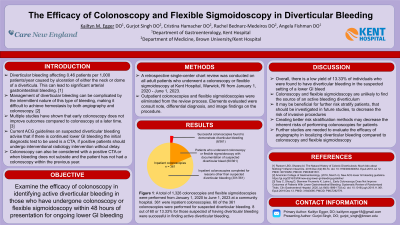
Results: A total of 1,326 colonoscopies and flexible sigmoidoscopies were performed between January 1, 2020 - June 1, 2023. A total of 27.22% (361/1,326) were performed on inpatients. A total of 16.62% (60/361) had undergone colonoscopy or flexible sigmoidoscopy with documentation of lower GI bleeding from a suspected diverticular source. Only 13.33% (8/60) were successful in finding active bleeding diverticulosis.
Discussion: Colonoscopy and Flexible sigmoidoscopy are unlikely to find the source of an active bleeding diverticulum, despite ongoing lower GI bleeding. Further studies are needed to evaluate the efficacy of angiography in localizing diverticular bleeding compared to colonoscopy and flexible sigmoidoscopy.
Disclosures:
Kailtyn M. Egger, DO1, Gurjot Singh, DO2, Cristina Hamacher, DO1, Rachel Bednarz-Medeiros, DO3, Angela Fishman, DO4. P2454 - The Efficacy of Colonoscopy and Flexible Sigmoidoscopy in Diverticular Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kent Hospital, Warwick, RI; 2The Warren Alpert Medical School of Brown University, Warwick, RI; 3Brown University / Warren Alpert Medical School, Warwick, RI; 4University Gastroenterology, East Greenwich, RI
Introduction: Diverticular bleeding affecting 0.46 patients per 1,000 patients/year caused by ulceration of either the neck or dome of a diverticula, can lead to significant arterial gastrointestinal bleeding. Management of diverticular bleeding can be complicated by the intermittent nature of this type of bleeding, making it difficult to achieve hemostasis by both angiography and colonoscopy. Multiple studies have shown that early colonoscopy does not improve outcomes compared to colonoscopy at a later. Therefore, the current American College of Gastroenterology guidelines on suspected diverticular bleeding advise that if there is continued lower GI bleeding the initial diagnostic test to be used is a CTA, if positive patients should undergo interventional radiology intervention without delay. Colonoscopy can also be considered with a positive CTA or when bleeding does not subside and the patient has not had a colonoscopy within the previous year. In this project, I examine the efficacy of colonoscopy in identifying active diverticular bleeding in those who have undergone colonoscopy or flexible sigmoidoscopy within 48 hours of presentation for ongoing lower GI bleeding.
Methods: A retrospective single-center chart review was conducted on all adult patients who underwent a colonoscopy or flexible sigmoidoscopy at Kent Hospital, Warwick, RI from January 1, 2020 - June 1, 2023. Outpatient colonoscopies and flexible sigmoidoscopies were eliminated from the review process. Elements evaluated were consult note differential diagnosis and findings on the procedure.
Results: A total of 1,326 colonoscopies and flexible sigmoidoscopies were performed between January 1, 2020 - June 1, 2023. A total of 27.22% (361/1,326) were performed on inpatients. A total of 16.62% (60/361) had undergone colonoscopy or flexible sigmoidoscopy with documentation of lower GI bleeding from a suspected diverticular source. Only 13.33% (8/60) were successful in finding active bleeding diverticulosis.
Discussion: Colonoscopy and Flexible sigmoidoscopy are unlikely to find the source of an active bleeding diverticulum, despite ongoing lower GI bleeding. Further studies are needed to evaluate the efficacy of angiography in localizing diverticular bleeding compared to colonoscopy and flexible sigmoidoscopy.
Disclosures:
Kailtyn Egger indicated no relevant financial relationships.
Gurjot Singh indicated no relevant financial relationships.
Cristina Hamacher indicated no relevant financial relationships.
Rachel Bednarz-Medeiros indicated no relevant financial relationships.
Angela Fishman indicated no relevant financial relationships.
Kailtyn M. Egger, DO1, Gurjot Singh, DO2, Cristina Hamacher, DO1, Rachel Bednarz-Medeiros, DO3, Angela Fishman, DO4. P2454 - The Efficacy of Colonoscopy and Flexible Sigmoidoscopy in Diverticular Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
