Monday Poster Session
Category: General Endoscopy
P2380 - Experience and Outcomes of Virtual Reality Prior to Routine Endoscopic Procedures
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- EV
Elida Voth, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Elida Voth, MD, Anjali Rajagopal, MBBS, Cayden Kleven, , Miranda Hamlin, MA, Benjamin Groteboer, RN, Julie Armenta, MSN, RN, Xiao Jing (Iris) Wang, MD
Mayo Clinic, Rochester, MN
Introduction: Esophagogastroduodenoscopy (EGD) and colonoscopy, while generally well-tolerated, can range from unpleasant to painful for patients. Rarely, the procedure must be terminated prematurely due to pain despite sedation, which wastes healthcare resources, leads to patient dissatisfaction and potentially decreases future compliance. Virtual reality (VR) can be used to help self-regulate anxiety and induce positive mood changes. The potential efficacy of VR as an adjunct to sedation medications to improve procedural tolerance is not well studied. We aimed to investigate whether the use of a VR device prior to elective outpatient endoscopy has an effect on patient’s perceived pre-procedural anxiety, clinical measures and procedural success.
Methods: Patients were offered use of a handheld VR device (Healium) in the pre-procedure area. The State Trait Anxiety Inventory (STAI) Score was completed before and after use of the VR device. Vital signs were obtained before VR, immediately prior to the procedure and prior to any initiation of sedative medications. Patient characteristics such as age, gender, prior psychiatric diagnoses, pertinent medication use, and history of prior endoscopic procedures were recorded along with amount of sedation administered and procedural completion. Descriptive statistics and a t-test were utilized for statistical analysis.
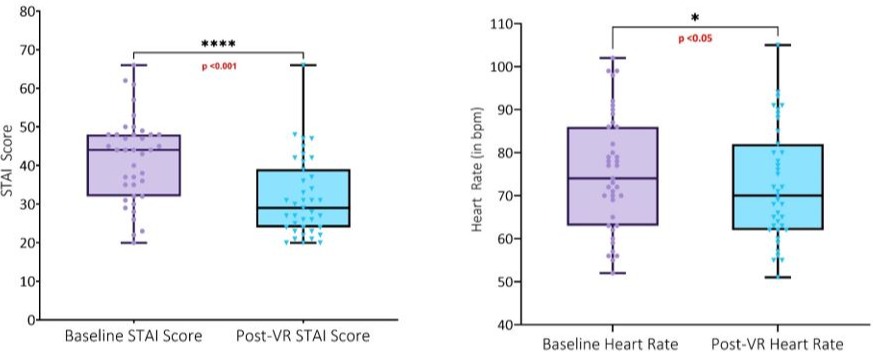
Results: There were 39 patients (56% female; mean age 48 years) included undergoing EGD (25%), colonoscopy (64%), and EGD/colonoscopy combination (10%). Comorbidities included anxiety (46.2%), depression (53.8%), PTSD (2.6%), and others (i.e. bipolar disorder) in (10% ) of participants. Medication use included SSRI/SNRI (21%), benzodiazepine (10.5%), prescription sleep aid (13.2%), or other anxiolytic/antidepressant (18.4%) [Table 1]. VR was most used during IV placement (61.5%) and for a mean duration of 4.6 mins. The mean baseline HR was 75.3 compared to 72.5 post-VR (p = 0.02). The mean baseline STAI score was 41.6, compared to 31.6 post- VR (p < 0.001). All procedures were completed, with 97% well tolerated [Figure 1]. Qualitative feedback was positive towards VR use, particularly for IV insertion.
Discussion: Our study suggests VR may be an effective non-pharmacologic tool to reduce procedure-related anxiety, which may result in improved patient satisfaction and procedural tolerability. Future studies are needed to better characterize the optimal use of these tools and their clinical impact.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elida Voth, MD, Anjali Rajagopal, MBBS, Cayden Kleven, , Miranda Hamlin, MA, Benjamin Groteboer, RN, Julie Armenta, MSN, RN, Xiao Jing (Iris) Wang, MD. P2380 - Experience and Outcomes of Virtual Reality Prior to Routine Endoscopic Procedures, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Esophagogastroduodenoscopy (EGD) and colonoscopy, while generally well-tolerated, can range from unpleasant to painful for patients. Rarely, the procedure must be terminated prematurely due to pain despite sedation, which wastes healthcare resources, leads to patient dissatisfaction and potentially decreases future compliance. Virtual reality (VR) can be used to help self-regulate anxiety and induce positive mood changes. The potential efficacy of VR as an adjunct to sedation medications to improve procedural tolerance is not well studied. We aimed to investigate whether the use of a VR device prior to elective outpatient endoscopy has an effect on patient’s perceived pre-procedural anxiety, clinical measures and procedural success.
Methods: Patients were offered use of a handheld VR device (Healium) in the pre-procedure area. The State Trait Anxiety Inventory (STAI) Score was completed before and after use of the VR device. Vital signs were obtained before VR, immediately prior to the procedure and prior to any initiation of sedative medications. Patient characteristics such as age, gender, prior psychiatric diagnoses, pertinent medication use, and history of prior endoscopic procedures were recorded along with amount of sedation administered and procedural completion. Descriptive statistics and a t-test were utilized for statistical analysis.
Results: There were 39 patients (56% female; mean age 48 years) included undergoing EGD (25%), colonoscopy (64%), and EGD/colonoscopy combination (10%). Comorbidities included anxiety (46.2%), depression (53.8%), PTSD (2.6%), and others (i.e. bipolar disorder) in (10% ) of participants. Medication use included SSRI/SNRI (21%), benzodiazepine (10.5%), prescription sleep aid (13.2%), or other anxiolytic/antidepressant (18.4%) [Table 1]. VR was most used during IV placement (61.5%) and for a mean duration of 4.6 mins. The mean baseline HR was 75.3 compared to 72.5 post-VR (p = 0.02). The mean baseline STAI score was 41.6, compared to 31.6 post- VR (p < 0.001). All procedures were completed, with 97% well tolerated [Figure 1]. Qualitative feedback was positive towards VR use, particularly for IV insertion.
Discussion: Our study suggests VR may be an effective non-pharmacologic tool to reduce procedure-related anxiety, which may result in improved patient satisfaction and procedural tolerability. Future studies are needed to better characterize the optimal use of these tools and their clinical impact.
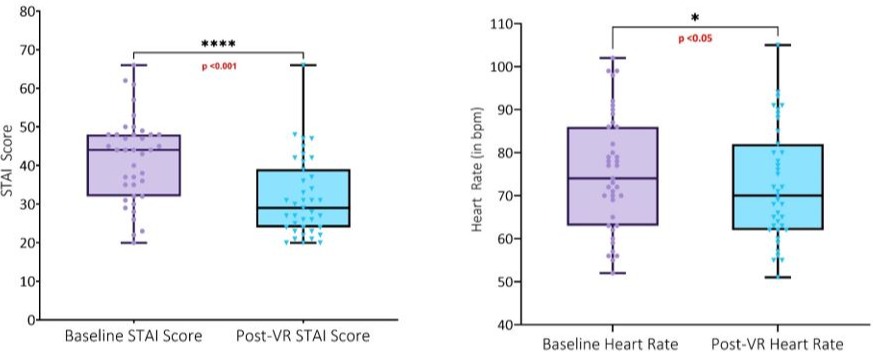
Figure: Baseline and Post-VR assessment of State Trait Anxiety Inventory and Heart Rate
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elida Voth indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
Cayden Kleven indicated no relevant financial relationships.
Miranda Hamlin indicated no relevant financial relationships.
Benjamin Groteboer indicated no relevant financial relationships.
Julie Armenta indicated no relevant financial relationships.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Elida Voth, MD, Anjali Rajagopal, MBBS, Cayden Kleven, , Miranda Hamlin, MA, Benjamin Groteboer, RN, Julie Armenta, MSN, RN, Xiao Jing (Iris) Wang, MD. P2380 - Experience and Outcomes of Virtual Reality Prior to Routine Endoscopic Procedures, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
