Monday Poster Session
Category: General Endoscopy
P2386 - Improving Inpatient Workflow and Optimizing Resource Utilization in the Endoscopy Unit in a Tertiary Care Center
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Neil Nadpara, MD
Stony Brook Medicine
Ronkonkoma, NY
Presenting Author(s)
Neil Nadpara, MD1, Jonathan Steinberg, MD1, Sandy Ng, MD1, Hong Gi Shim, MD2, Lionel D'Souza, MD1
1Stony Brook Medicine, Stony Brook, NY; 2Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Delays in performing inpatient procedures may lead to inefficient resource utilization and poor patient experience. While patient factors are often unpredictable and more difficult to address, targeted systems interventions may prevent procedural delays. Our aim was to evaluate if dedicated procedural block time and preemptive anesthesia assessment improved the efficiency of the inpatient endoscopy workflow.
Methods: Baseline daily inpatient case completion rate, patient demographics, and procedure characteristics were obtained via retrospective chart review of cases performed from July 2022 to February 2023. Using a Plan-Do-Study-Act cycle, two interventions were designed: a dedicated 4-hour block for inpatient procedures each weekday (morning or afternoon) and an anesthesia consultation service to evaluate patients deemed at higher risk for adverse events. Data was then collected prospectively from March 2023 to September 2023. We established a target daily case completion rate of 90% and final procedure end time of 6 PM.
Results: Patient and procedure characteristics for delayed cases were similar between the pre-and post-intervention groups (Table 1). In both groups, the most common reason for procedural delay was inadequate bowel prep (32% vs. 40%, p = 0.23). A similar proportion of cases were delayed due to lack of endoscopy unit resources (19% vs. 14%, p = 0.37) or incomplete pre-procedure assessment (5% vs. 3%, p = 0.60).
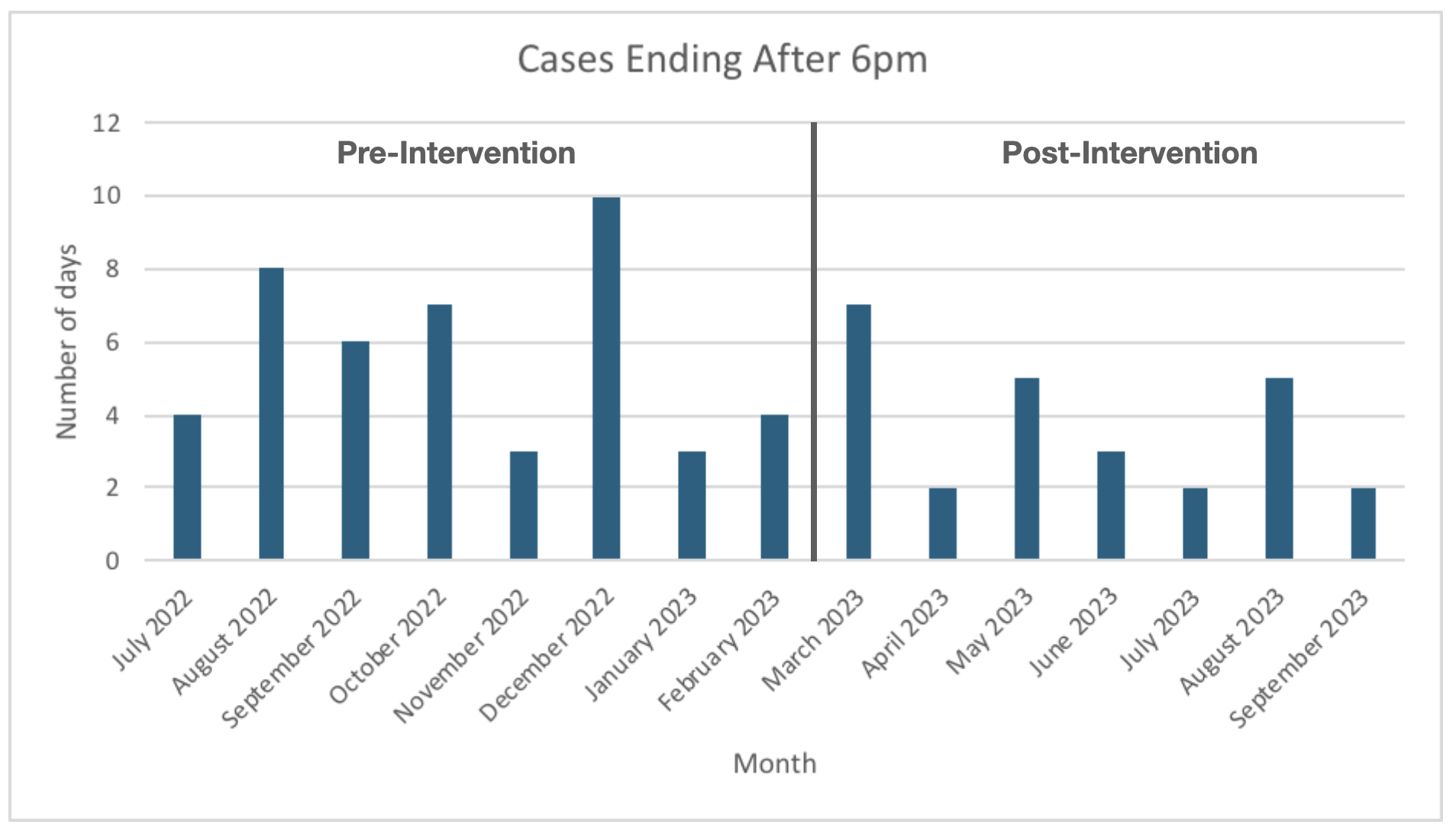
The average daily case completion rates (79.1% vs. 79.2%) and percentage of delayed cases each month (21.5% vs. 23.0%) were comparable for the two groups. There were fewer days per month where cases ended after 6 PM in the post-intervention group (5.75 vs. 3.71, p = 0.10, Figure 1). While case completion rates for morning and afternoon block times in the post-intervention group were similar, a smaller proportion of cases started after 5 PM when a morning block was assigned (15% vs. 27%, p = 0.25).
Discussion: While there was no significant difference in the average daily case completion rate between the pre- and post-intervention groups, the interventions led to a decrease in the number of days with cases ending after 6 PM, suggesting improved efficiency for inpatient procedures. Our findings also suggest that certain patient factors (inadequate bowel prep and changes in clinical status) may be bigger drivers of procedure delays than system factors. Tailoring interventions to improve these patient-related events may further enhance inpatient procedure efficiency.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neil Nadpara, MD1, Jonathan Steinberg, MD1, Sandy Ng, MD1, Hong Gi Shim, MD2, Lionel D'Souza, MD1. P2386 - Improving Inpatient Workflow and Optimizing Resource Utilization in the Endoscopy Unit in a Tertiary Care Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stony Brook Medicine, Stony Brook, NY; 2Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Delays in performing inpatient procedures may lead to inefficient resource utilization and poor patient experience. While patient factors are often unpredictable and more difficult to address, targeted systems interventions may prevent procedural delays. Our aim was to evaluate if dedicated procedural block time and preemptive anesthesia assessment improved the efficiency of the inpatient endoscopy workflow.
Methods: Baseline daily inpatient case completion rate, patient demographics, and procedure characteristics were obtained via retrospective chart review of cases performed from July 2022 to February 2023. Using a Plan-Do-Study-Act cycle, two interventions were designed: a dedicated 4-hour block for inpatient procedures each weekday (morning or afternoon) and an anesthesia consultation service to evaluate patients deemed at higher risk for adverse events. Data was then collected prospectively from March 2023 to September 2023. We established a target daily case completion rate of 90% and final procedure end time of 6 PM.
Results: Patient and procedure characteristics for delayed cases were similar between the pre-and post-intervention groups (Table 1). In both groups, the most common reason for procedural delay was inadequate bowel prep (32% vs. 40%, p = 0.23). A similar proportion of cases were delayed due to lack of endoscopy unit resources (19% vs. 14%, p = 0.37) or incomplete pre-procedure assessment (5% vs. 3%, p = 0.60).
The average daily case completion rates (79.1% vs. 79.2%) and percentage of delayed cases each month (21.5% vs. 23.0%) were comparable for the two groups. There were fewer days per month where cases ended after 6 PM in the post-intervention group (5.75 vs. 3.71, p = 0.10, Figure 1). While case completion rates for morning and afternoon block times in the post-intervention group were similar, a smaller proportion of cases started after 5 PM when a morning block was assigned (15% vs. 27%, p = 0.25).
Discussion: While there was no significant difference in the average daily case completion rate between the pre- and post-intervention groups, the interventions led to a decrease in the number of days with cases ending after 6 PM, suggesting improved efficiency for inpatient procedures. Our findings also suggest that certain patient factors (inadequate bowel prep and changes in clinical status) may be bigger drivers of procedure delays than system factors. Tailoring interventions to improve these patient-related events may further enhance inpatient procedure efficiency.
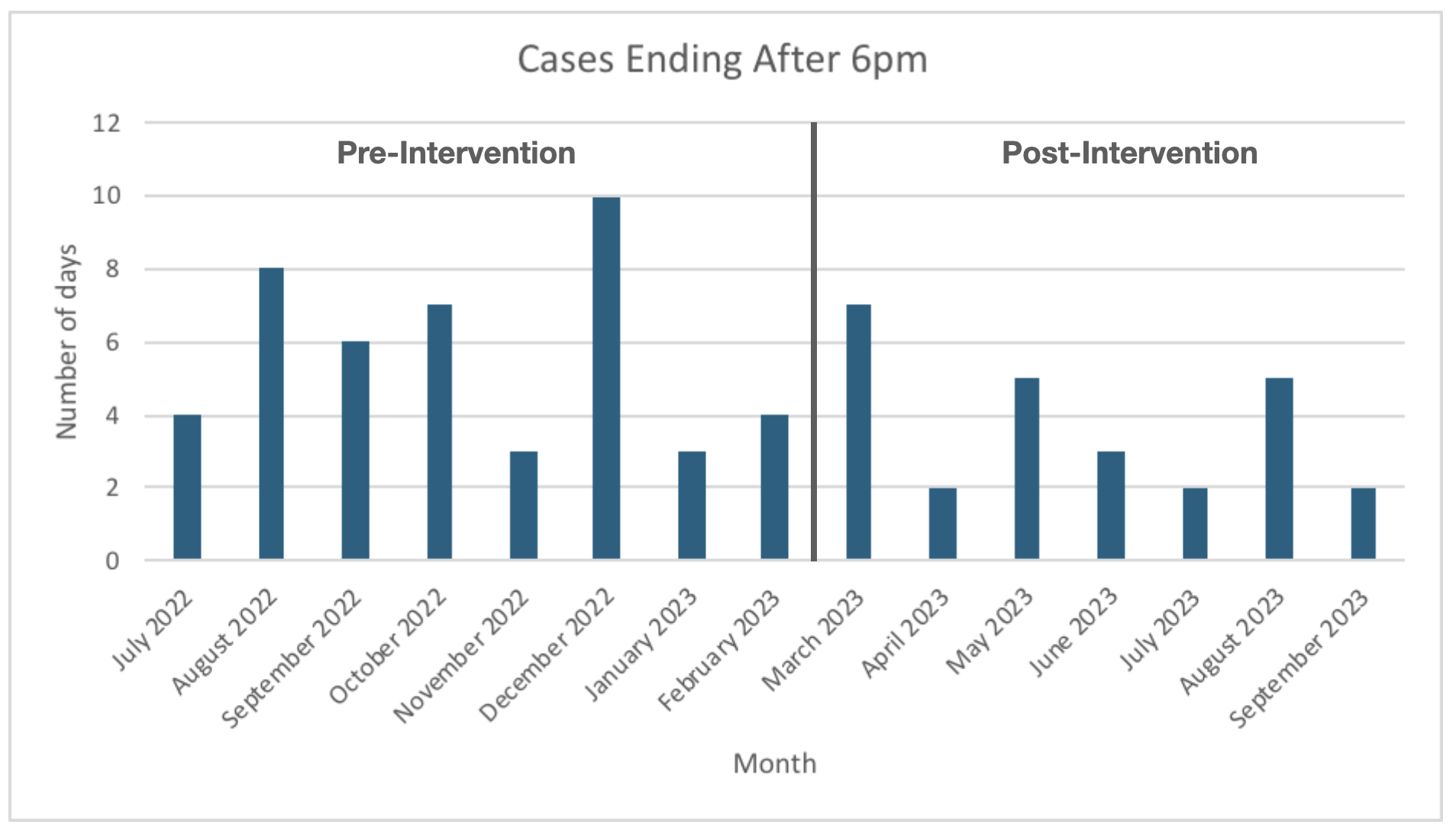
Figure: Number of cases ending after 6pm each month in the pre-Intervention and post-Intervention groups
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neil Nadpara indicated no relevant financial relationships.
Jonathan Steinberg indicated no relevant financial relationships.
Sandy Ng indicated no relevant financial relationships.
Hong Gi Shim indicated no relevant financial relationships.
Lionel D'Souza indicated no relevant financial relationships.
Neil Nadpara, MD1, Jonathan Steinberg, MD1, Sandy Ng, MD1, Hong Gi Shim, MD2, Lionel D'Souza, MD1. P2386 - Improving Inpatient Workflow and Optimizing Resource Utilization in the Endoscopy Unit in a Tertiary Care Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
