Monday Poster Session
Category: General Endoscopy
P2390 - Outcomes and Complications in Patients With Stimulant Abuse, Admitted for NVUGIB: A 2016-2020 United States National Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Al Smadi, MD
University of California Riverside School of Medicine
San Bernardino, CA
Presenting Author(s)
Khaled Al Smadi, MD1, Miguel J. Salazar, MD2, Pedro Palacios, MD3, Do Han Kim, MD4, Ko Dong, MD5, Gianina Flocco, MD6, George Saffouri, MD7, Harold Paredes, MD7
1University of California Riverside School of Medicine, San Bernardino, CA; 2University of California Riverside, Rancho Cucamonga, CA; 3Mayo Clinic, Jacksonville, FL; 4Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 5Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 6Cleveland Clinic, Cleveland, OH; 7University of California Riverside, Rialto, CA
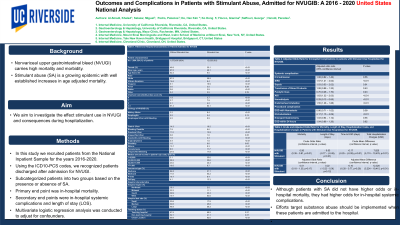
Introduction: Nonvariceal upper gastrointestinal bleed (NVUGI) carries high mortality and morbidity. Stimulant abuse (SA) is a growing epidemic with well established increases in age adjusted mortality. SA has been reported as a potential cause of serious GI complications, and outcomes in anesthesia have demonstrated higher risk for adverse events including mortality. Accordingly, we aim to investigate the effect stimulant use in NVUGI and consequences during hospitalization.
Methods: In this study we recruited patients from the National Inpatient Sample for the years 2016-2020. Using the ICD10-PCS codes, we recognized patients discharged after admission for NVUGI then divided them into two groups based on the presence or absence of SA. The primary end point was in-hospital mortality while secondary end points were in-hospital systemic complications, length of stay (LOS) and healthcare related charges and costs. Multivariate logistic regression analysis was conducted to adjust for confounders.
Results: A total of 1,984,524 patients with discharges after NVUGI were identified out of which 12,029 (0.6%) had associated SA. Mallory Weiss tear was the most likely cause of GI bleed (6.4% vs.3.2%; p< 0.01), also higher rates of esophageal, gastric and duodenal ulcers (9.9%vs.4.5%, 16.2%vs. 4.3%, 13.9%vs.11.2%; p< 0.01). They were less likely females (30.1%vs.46.9%; p< 0.01) and more likely younger (mean age 49.1vs.67.5; p< 0.01), with predominant White race in both groups (58.9%vs.67.5%; p< 0.01) and more Hispanics among SA group (19.9%vs.9.1%; p< 0.01). SA had higher rates of OH abuse (42.9%vs.12.6%, p< 0,01), cannabis abuse (20.9%vs.1.7%; p< 0.01), opiate abuse (13.9%vs.1.4%; p< 0.01) and tobacco abuse (2.7%vs.0.9%; p< 0.01). After adjusting for confounders patients with SA they had higher odds for SIRS (1.57, CI 1.21–2.02; p< 0.01), AKI (1.63, CI 1.32–2.03; p< 0.01), hemodialysis (0.29, CI 0.13–0.65; p< 0.01), endotracheal intubation (1.55, CI 1.28–1.88; p< 0.01) and need for IR-embolization (2.17, CI 1.15–4.09; p< 0.01). They did not have increased risk for mortality (0.51, CI 0.18–1.35; p=0.17), prolonged LOS or delay in EGD (-0.01, CI -0.28–0.77; p=0.26) but had higher hospital charges CI 12,320, CI 5,224–19,415; p< 0.01).
Discussion: Although patients with SA did not have higher odds for in-hospital mortality, they had higher odds for in-hospital systemic complications. Efforts to target substance abuse should be implemented when these patients are admitted to the hospital.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Al Smadi, MD1, Miguel J. Salazar, MD2, Pedro Palacios, MD3, Do Han Kim, MD4, Ko Dong, MD5, Gianina Flocco, MD6, George Saffouri, MD7, Harold Paredes, MD7. P2390 - Outcomes and Complications in Patients With Stimulant Abuse, Admitted for NVUGIB: A 2016-2020 United States National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Riverside School of Medicine, San Bernardino, CA; 2University of California Riverside, Rancho Cucamonga, CA; 3Mayo Clinic, Jacksonville, FL; 4Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 5Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 6Cleveland Clinic, Cleveland, OH; 7University of California Riverside, Rialto, CA
Introduction: Nonvariceal upper gastrointestinal bleed (NVUGI) carries high mortality and morbidity. Stimulant abuse (SA) is a growing epidemic with well established increases in age adjusted mortality. SA has been reported as a potential cause of serious GI complications, and outcomes in anesthesia have demonstrated higher risk for adverse events including mortality. Accordingly, we aim to investigate the effect stimulant use in NVUGI and consequences during hospitalization.
Methods: In this study we recruited patients from the National Inpatient Sample for the years 2016-2020. Using the ICD10-PCS codes, we recognized patients discharged after admission for NVUGI then divided them into two groups based on the presence or absence of SA. The primary end point was in-hospital mortality while secondary end points were in-hospital systemic complications, length of stay (LOS) and healthcare related charges and costs. Multivariate logistic regression analysis was conducted to adjust for confounders.
Results: A total of 1,984,524 patients with discharges after NVUGI were identified out of which 12,029 (0.6%) had associated SA. Mallory Weiss tear was the most likely cause of GI bleed (6.4% vs.3.2%; p< 0.01), also higher rates of esophageal, gastric and duodenal ulcers (9.9%vs.4.5%, 16.2%vs. 4.3%, 13.9%vs.11.2%; p< 0.01). They were less likely females (30.1%vs.46.9%; p< 0.01) and more likely younger (mean age 49.1vs.67.5; p< 0.01), with predominant White race in both groups (58.9%vs.67.5%; p< 0.01) and more Hispanics among SA group (19.9%vs.9.1%; p< 0.01). SA had higher rates of OH abuse (42.9%vs.12.6%, p< 0,01), cannabis abuse (20.9%vs.1.7%; p< 0.01), opiate abuse (13.9%vs.1.4%; p< 0.01) and tobacco abuse (2.7%vs.0.9%; p< 0.01). After adjusting for confounders patients with SA they had higher odds for SIRS (1.57, CI 1.21–2.02; p< 0.01), AKI (1.63, CI 1.32–2.03; p< 0.01), hemodialysis (0.29, CI 0.13–0.65; p< 0.01), endotracheal intubation (1.55, CI 1.28–1.88; p< 0.01) and need for IR-embolization (2.17, CI 1.15–4.09; p< 0.01). They did not have increased risk for mortality (0.51, CI 0.18–1.35; p=0.17), prolonged LOS or delay in EGD (-0.01, CI -0.28–0.77; p=0.26) but had higher hospital charges CI 12,320, CI 5,224–19,415; p< 0.01).
Discussion: Although patients with SA did not have higher odds for in-hospital mortality, they had higher odds for in-hospital systemic complications. Efforts to target substance abuse should be implemented when these patients are admitted to the hospital.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Al Smadi indicated no relevant financial relationships.
Miguel Salazar indicated no relevant financial relationships.
Pedro Palacios indicated no relevant financial relationships.
Do Han Kim indicated no relevant financial relationships.
Ko Dong indicated no relevant financial relationships.
Gianina Flocco indicated no relevant financial relationships.
George Saffouri indicated no relevant financial relationships.
Harold Paredes indicated no relevant financial relationships.
Khaled Al Smadi, MD1, Miguel J. Salazar, MD2, Pedro Palacios, MD3, Do Han Kim, MD4, Ko Dong, MD5, Gianina Flocco, MD6, George Saffouri, MD7, Harold Paredes, MD7. P2390 - Outcomes and Complications in Patients With Stimulant Abuse, Admitted for NVUGIB: A 2016-2020 United States National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
