Monday Poster Session
Category: General Endoscopy
P2393 - Impact of GLP-1 Agonist Versus Opioid Use on Esophagogastroduodenoscopy (EGD) Outcomes: A Propensity-Matched Analysis of the U.S. Collaborative Network
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mouhand F.H Mohamed, MD, MSc
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Osama Hamid, MD3, Khaled Elfert, MD4, Mohanad Awadalla, MD5, Indira Bhavsar-Burke, MD, MHPE3, John Guardiola, MD2
1Mayo Clinic, Rochester, MN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Texas Southwestern Medical Center, Dallas, TX; 4West Virginia University, Morgantown, WV; 5Beth Israel Deaconess Medical Center, Boston, MA
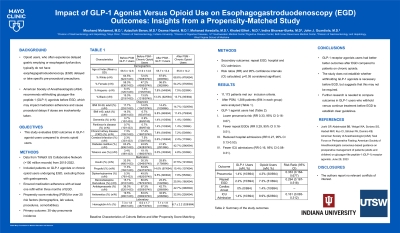
Introduction: Opioid users often have delayed gastric emptying or esophageal dysfunction but usually do not have esophagogastroduodenoscopy (EGD) delayed or receive specific pre-procedural precautions. Users of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are advised to withhold the medication before EGD per American Society of Anesthesiologists recommendations. This may impact medication adherence and lead to procedural delays if doses are taken. Our study aims to evaluate EGD outcomes in patients treated with GLP-1 RAs compared to chronic opioids.
Methods: We utilized the TriNetX US Collaborative Network Database, including > 100 million patient records. We selected patients who underwent EGD from 2015 to 2022 and compared those taking GLP-1 RAs with those maintained on long-term opiates. Patients with gastroparesis were excluded. To ensure medication adherence, both groups had confirmed medication refills within three months of the EGD. Propensity score matching (PSM) accounting for over 25 risk factors, including demographics, laboratory values, procedures, and comorbid conditions, was performed. The primary outcome was the 30-day incidence of pneumonia. We also assessed the need for repeat EGD, ICU admission, and respiratory failure. Risk ratios (RR) and 95% confidence intervals (CI) were used for comparison. A p-value < 0.05 was considered statistically significant.
Results: 11,173 patients met inclusion criteria. After PSM, 1,388 patients (694 in each group) were analyzed. Baseline characteristics of each cohort are summarized in Table 1. Compared to patients on chronic opioids, patients on GLP-1 RAs had lower rates of pneumonia [RR 0.33 95% CI (0.16-0.67)], repeat EGD [RR 0.29 95% CI (0.16-0.51)], hospital admission [RR 0.27 95% CI (0.13-0.53)], and ICU admission [RR 0.16 95% CI (0.08-0.31)] (Table 2).
Discussion: Results from this database analysis suggest that GLP-1 RA use is associated with better outcomes compared to long-term opioid use after EGD. While this study does not resolve the ongoing debate regarding the safety of GLP1-RAs in patients undergoing EGD, it does provide useful information to currently available data. Our data provides reassurance that outcomes in patients receiving GLP1-RAs are not worse compared to a control group of patients at risk for medication-induced delayed gastric emptying. Withholding GLP-1 RAs may not be necessary before EGD. Further research in outcomes of patients receiving GLP1-RAs is essential to establish definitive guidelines.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Osama Hamid, MD3, Khaled Elfert, MD4, Mohanad Awadalla, MD5, Indira Bhavsar-Burke, MD, MHPE3, John Guardiola, MD2. P2393 - Impact of GLP-1 Agonist Versus Opioid Use on Esophagogastroduodenoscopy (EGD) Outcomes: A Propensity-Matched Analysis of the U.S. Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Texas Southwestern Medical Center, Dallas, TX; 4West Virginia University, Morgantown, WV; 5Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Opioid users often have delayed gastric emptying or esophageal dysfunction but usually do not have esophagogastroduodenoscopy (EGD) delayed or receive specific pre-procedural precautions. Users of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are advised to withhold the medication before EGD per American Society of Anesthesiologists recommendations. This may impact medication adherence and lead to procedural delays if doses are taken. Our study aims to evaluate EGD outcomes in patients treated with GLP-1 RAs compared to chronic opioids.
Methods: We utilized the TriNetX US Collaborative Network Database, including > 100 million patient records. We selected patients who underwent EGD from 2015 to 2022 and compared those taking GLP-1 RAs with those maintained on long-term opiates. Patients with gastroparesis were excluded. To ensure medication adherence, both groups had confirmed medication refills within three months of the EGD. Propensity score matching (PSM) accounting for over 25 risk factors, including demographics, laboratory values, procedures, and comorbid conditions, was performed. The primary outcome was the 30-day incidence of pneumonia. We also assessed the need for repeat EGD, ICU admission, and respiratory failure. Risk ratios (RR) and 95% confidence intervals (CI) were used for comparison. A p-value < 0.05 was considered statistically significant.
Results: 11,173 patients met inclusion criteria. After PSM, 1,388 patients (694 in each group) were analyzed. Baseline characteristics of each cohort are summarized in Table 1. Compared to patients on chronic opioids, patients on GLP-1 RAs had lower rates of pneumonia [RR 0.33 95% CI (0.16-0.67)], repeat EGD [RR 0.29 95% CI (0.16-0.51)], hospital admission [RR 0.27 95% CI (0.13-0.53)], and ICU admission [RR 0.16 95% CI (0.08-0.31)] (Table 2).
Discussion: Results from this database analysis suggest that GLP-1 RA use is associated with better outcomes compared to long-term opioid use after EGD. While this study does not resolve the ongoing debate regarding the safety of GLP1-RAs in patients undergoing EGD, it does provide useful information to currently available data. Our data provides reassurance that outcomes in patients receiving GLP1-RAs are not worse compared to a control group of patients at risk for medication-induced delayed gastric emptying. Withholding GLP-1 RAs may not be necessary before EGD. Further research in outcomes of patients receiving GLP1-RAs is essential to establish definitive guidelines.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand Mohamed indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Osama Hamid, MD3, Khaled Elfert, MD4, Mohanad Awadalla, MD5, Indira Bhavsar-Burke, MD, MHPE3, John Guardiola, MD2. P2393 - Impact of GLP-1 Agonist Versus Opioid Use on Esophagogastroduodenoscopy (EGD) Outcomes: A Propensity-Matched Analysis of the U.S. Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
