Monday Poster Session
Category: General Endoscopy
P2396 - Utilizing Anesthesia Risk to Reduce Delays in Endoscopy Case Completion
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NH
Nicholas Hebda, MD
University of Massachusetts Chan Medical School
Worcester, MA
Presenting Author(s)
Nicholas Hebda, MD1, Kimberly McGuigan, MBB2, Jeffrey Blackwell, 2, Jenna L'Heureux, NP3, Sarah M. Hyder, MD, MBA3, Christopher Marshall, MD3
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Health, Worcester, MA; 3University of Massachusetts Memorial Medical Center, Worcester, MA
Introduction: The volume of patients awaiting colonoscopy or upper endoscopy has increased over the last several years due to updated screening guidelines and back-logs related to the COVID-19 pandemic. Given a concurrent trend of increasing wait times for these procedures, minimizing delays and case cancelations can be a practical strategy to reduce waste.
Methods: In an attempt to reduce the number of late endoscopy cancellations at our institution due to need for medical clearance or higher level of anesthesia care, we developed an anesthesia risk-rating calculator within our electronic medical record which was implemented in January 2024. Medical co-morbidities that could inform risk of undergoing varying types of anesthesia (e.g., monitored anesthesia care vs. moderate sedation; see Table 1) were flagged, and patients ordered for colonoscopy or upper endoscopy were each assigned a numerical risk score. Scores were available for clinicians as well as schedulers at the time of scheduling in order to identify low-risk patients who were likely appropriate for either outpatient or in-hospital endoscopy suites, high-risk patients who required an operating room setting, and moderate risk patients who required further triage review prior to scheduling.
Results: Following implementation of our risk-rating scores, despite a higher case volume overall, the proportion of endoscopy cases canceled due to need for medical clearance or higher level of anesthesia care and subsequently rescheduled to a higher level of care decreased grossly by 10% from December 2023 (n=15/25) to May 2024 (n=11/22). In this same time frame, the proportion of cases canceled for one of these two reasons out of all cases canceled for a known reason and subsequently rescheduled to any level of care decreased by 5.4% (n=56/375 to n=39/410). There was also a statistically significant increase in the average number of days out from the original scheduled procedure that cases were being canceled for either medical clearance or need for higher level of anesthesia care from December to May after implementation of the risk-rating scores (19 vs. 32 days, p=0.043).
Discussion: Creation of an anesthesia risk-rating calculator within our electronic medical record has enabled a modest decrease in late endoscopy cancellations at our institution within several months of implementation. As our team becomes more consistent and sophisticated in the use of these risk ratings, we anticipate further reductions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nicholas Hebda, MD1, Kimberly McGuigan, MBB2, Jeffrey Blackwell, 2, Jenna L'Heureux, NP3, Sarah M. Hyder, MD, MBA3, Christopher Marshall, MD3. P2396 - Utilizing Anesthesia Risk to Reduce Delays in Endoscopy Case Completion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Health, Worcester, MA; 3University of Massachusetts Memorial Medical Center, Worcester, MA
Introduction: The volume of patients awaiting colonoscopy or upper endoscopy has increased over the last several years due to updated screening guidelines and back-logs related to the COVID-19 pandemic. Given a concurrent trend of increasing wait times for these procedures, minimizing delays and case cancelations can be a practical strategy to reduce waste.
Methods: In an attempt to reduce the number of late endoscopy cancellations at our institution due to need for medical clearance or higher level of anesthesia care, we developed an anesthesia risk-rating calculator within our electronic medical record which was implemented in January 2024. Medical co-morbidities that could inform risk of undergoing varying types of anesthesia (e.g., monitored anesthesia care vs. moderate sedation; see Table 1) were flagged, and patients ordered for colonoscopy or upper endoscopy were each assigned a numerical risk score. Scores were available for clinicians as well as schedulers at the time of scheduling in order to identify low-risk patients who were likely appropriate for either outpatient or in-hospital endoscopy suites, high-risk patients who required an operating room setting, and moderate risk patients who required further triage review prior to scheduling.
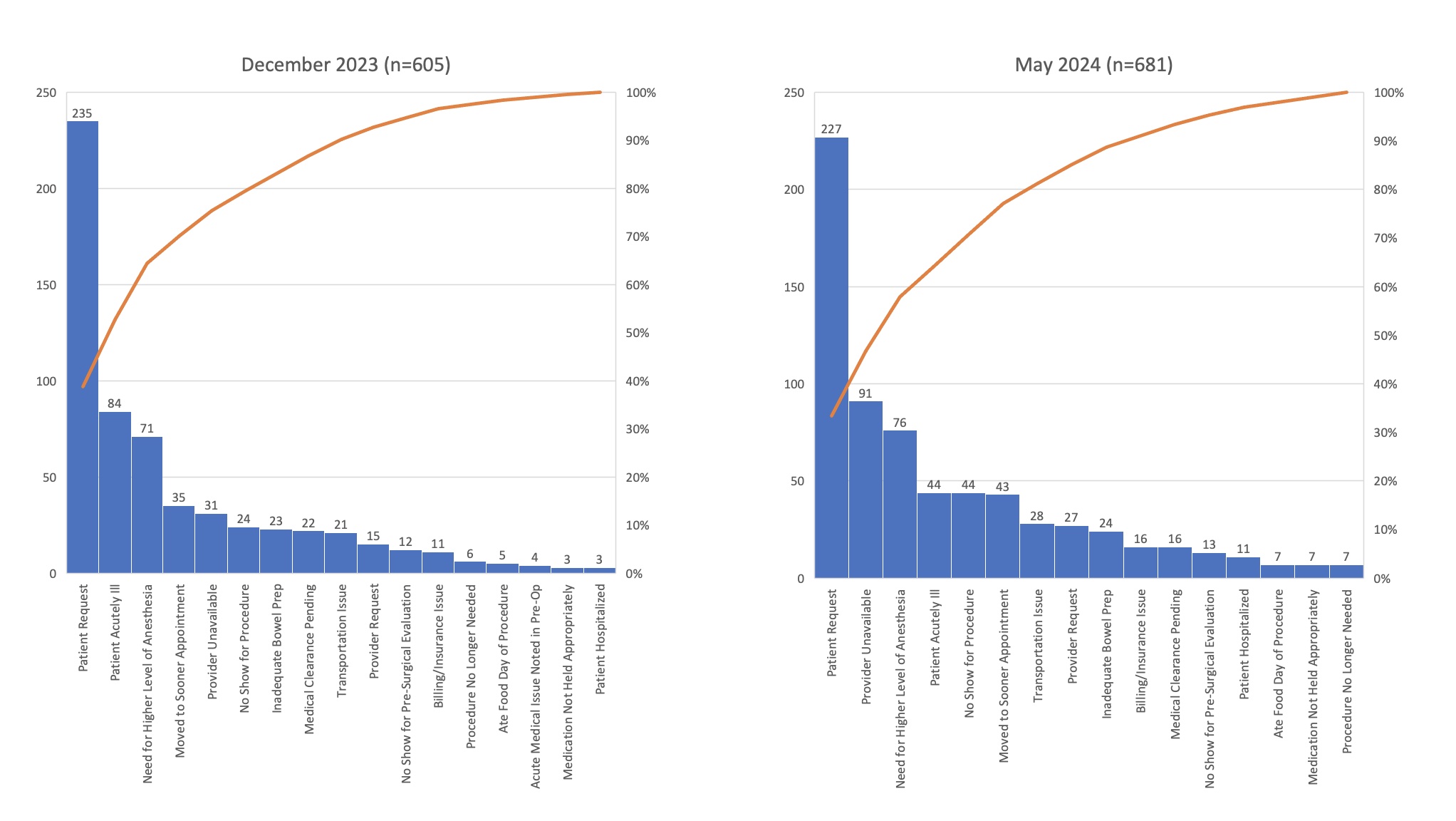
Results: Following implementation of our risk-rating scores, despite a higher case volume overall, the proportion of endoscopy cases canceled due to need for medical clearance or higher level of anesthesia care and subsequently rescheduled to a higher level of care decreased grossly by 10% from December 2023 (n=15/25) to May 2024 (n=11/22). In this same time frame, the proportion of cases canceled for one of these two reasons out of all cases canceled for a known reason and subsequently rescheduled to any level of care decreased by 5.4% (n=56/375 to n=39/410). There was also a statistically significant increase in the average number of days out from the original scheduled procedure that cases were being canceled for either medical clearance or need for higher level of anesthesia care from December to May after implementation of the risk-rating scores (19 vs. 32 days, p=0.043).
Discussion: Creation of an anesthesia risk-rating calculator within our electronic medical record has enabled a modest decrease in late endoscopy cancellations at our institution within several months of implementation. As our team becomes more consistent and sophisticated in the use of these risk ratings, we anticipate further reductions.
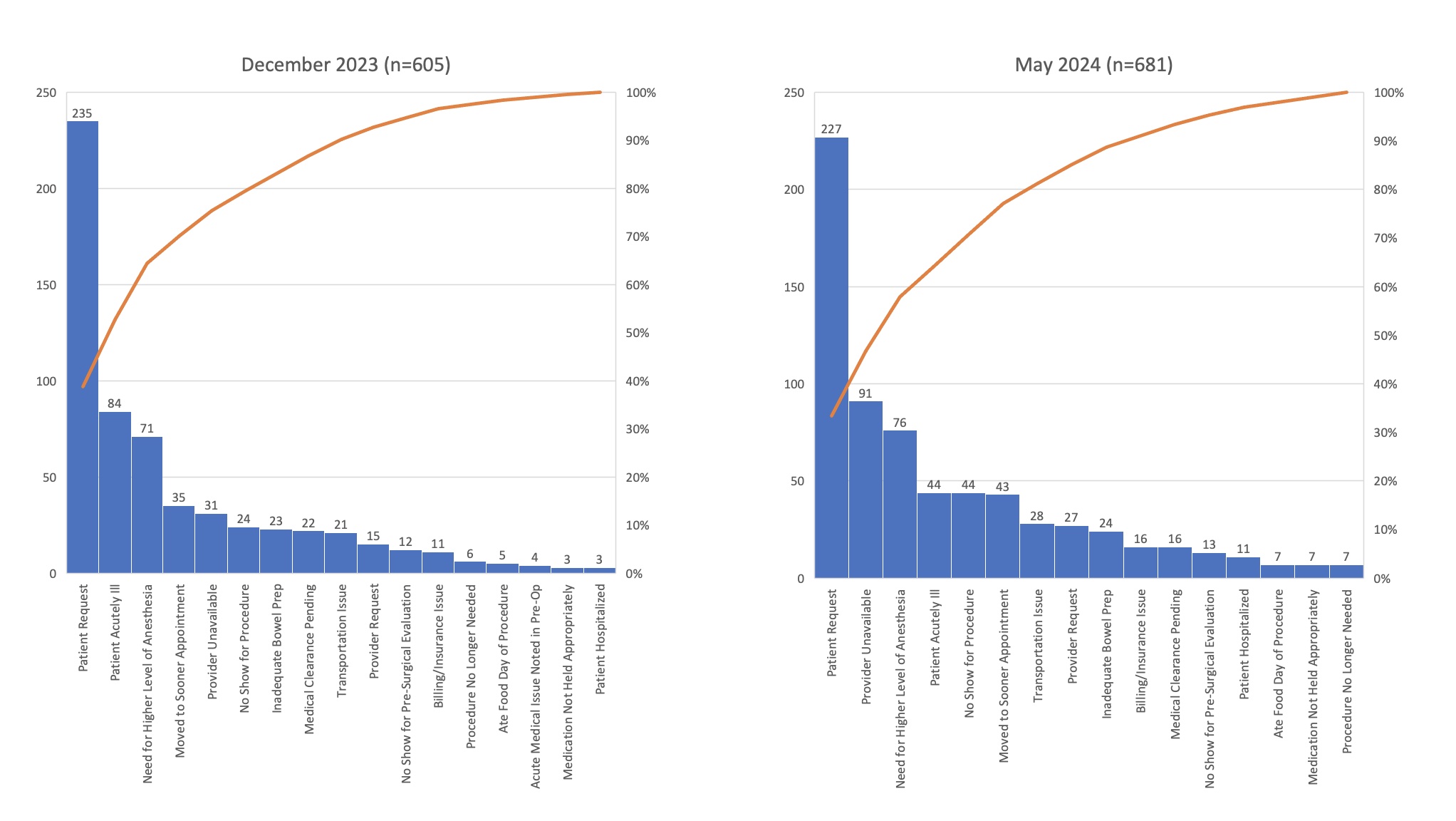
Figure: Figure 1. Case Cancellations for a Known Reason, December 2023 versus May 2024
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nicholas Hebda indicated no relevant financial relationships.
Kimberly McGuigan indicated no relevant financial relationships.
Jeffrey Blackwell indicated no relevant financial relationships.
Jenna L'Heureux indicated no relevant financial relationships.
Sarah Hyder indicated no relevant financial relationships.
Christopher Marshall indicated no relevant financial relationships.
Nicholas Hebda, MD1, Kimberly McGuigan, MBB2, Jeffrey Blackwell, 2, Jenna L'Heureux, NP3, Sarah M. Hyder, MD, MBA3, Christopher Marshall, MD3. P2396 - Utilizing Anesthesia Risk to Reduce Delays in Endoscopy Case Completion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

