Monday Poster Session
Category: Esophagus
P2306 - Endoscopic Findings of Necrotic Esophagus in the Setting of Suspected Malignancy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Arvind Bussetty, MD
Robert Wood Johnson Medical School, Rutgers University, NJ
Presenting Author(s)
Arvind Bussetty, MD, Toni Marie Chandler, MD, Keerthana Kesavarapu, MD
Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Esophageal necrosis is a rare condition associated with high morbidity and mortality. Typically, the mucosal findings are characterized by partial or circumferential black appearance which terminates at the gastroesophageal junction. It is commonly seen affecting the distal esophagus as it is susceptible to blood flow compromise. 80% of cases are appreciated in males, with a wide variety of associated risk factors. This condition can be life-threatening and it is important to recognize this condition during endoscopic evaluation. We would like to highlight a case to focus on the endoscopic findings of esophageal necrosis.
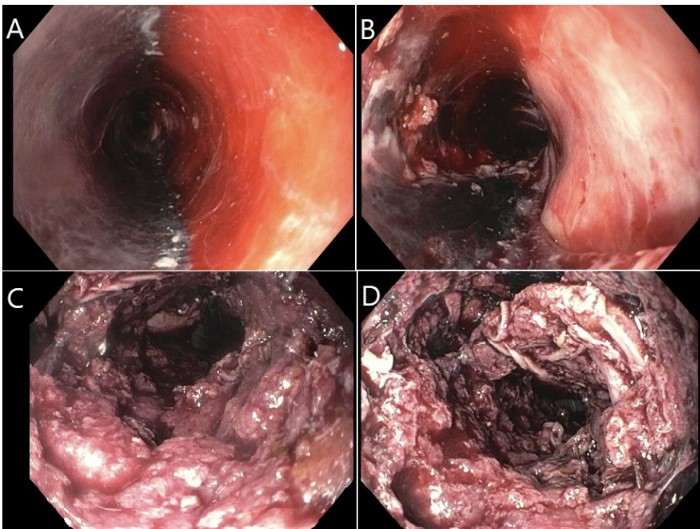
Case Description/Methods: We present an 86 year-old female with a past medical history of stroke, paroxysmal atrial fibrillation on eliquis, diastolic heart failure, hypertension, and chronic kidney disease admitted for hematemesis. On arrival, the patient was found to be disoriented and she was intubated to prevent airway compromise. Nasopharyngeal endoscopy was negative for a clear source. Upper endoscopy revealed necrotic and ischemic changes from the proximal to distal esophagus (Figure 1A and 1B) affecting 75% of the mucosa with severe circumferential debris that appeared to be eroding into the esophagus causing mucosal sloughing and active oozing of blood (Figure 1C and 1D). There was no evidence of gastric involvement. These findings were suspicious for malignancy. However, given that the patient would be a poor surgical or chemotherapy candidate, the family decided to pursue comfort measures rather than continue workup and further treatment.
Discussion: In cases of acute esophageal necrosis it is common to see hematemesis, melena and/or hemodynamic instability in males aged 60-80. It is thought to be caused by ischemic compromise due to the distal esophagus vulnerability to low-flow states. In this particular case, we particularly aim to highlight the endoscopic findings which showed mucosal sloughing and ischemic changes in a female patient. Unfortunately, there is limited data on appropriate management aside from parenteral nutrition, fluid resuscitation, proton pump inhibitors, blood transfusions, decompression, antibiotics when clinically indicated, and surgery in setting of perforation. Although prognosis is poor, it is important to be familiar with the endoscopic characteristics in order to diagnose and consider next steps appropriately.
Disclosures:
Arvind Bussetty, MD, Toni Marie Chandler, MD, Keerthana Kesavarapu, MD. P2306 - Endoscopic Findings of Necrotic Esophagus in the Setting of Suspected Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Esophageal necrosis is a rare condition associated with high morbidity and mortality. Typically, the mucosal findings are characterized by partial or circumferential black appearance which terminates at the gastroesophageal junction. It is commonly seen affecting the distal esophagus as it is susceptible to blood flow compromise. 80% of cases are appreciated in males, with a wide variety of associated risk factors. This condition can be life-threatening and it is important to recognize this condition during endoscopic evaluation. We would like to highlight a case to focus on the endoscopic findings of esophageal necrosis.
Case Description/Methods: We present an 86 year-old female with a past medical history of stroke, paroxysmal atrial fibrillation on eliquis, diastolic heart failure, hypertension, and chronic kidney disease admitted for hematemesis. On arrival, the patient was found to be disoriented and she was intubated to prevent airway compromise. Nasopharyngeal endoscopy was negative for a clear source. Upper endoscopy revealed necrotic and ischemic changes from the proximal to distal esophagus (Figure 1A and 1B) affecting 75% of the mucosa with severe circumferential debris that appeared to be eroding into the esophagus causing mucosal sloughing and active oozing of blood (Figure 1C and 1D). There was no evidence of gastric involvement. These findings were suspicious for malignancy. However, given that the patient would be a poor surgical or chemotherapy candidate, the family decided to pursue comfort measures rather than continue workup and further treatment.
Discussion: In cases of acute esophageal necrosis it is common to see hematemesis, melena and/or hemodynamic instability in males aged 60-80. It is thought to be caused by ischemic compromise due to the distal esophagus vulnerability to low-flow states. In this particular case, we particularly aim to highlight the endoscopic findings which showed mucosal sloughing and ischemic changes in a female patient. Unfortunately, there is limited data on appropriate management aside from parenteral nutrition, fluid resuscitation, proton pump inhibitors, blood transfusions, decompression, antibiotics when clinically indicated, and surgery in setting of perforation. Although prognosis is poor, it is important to be familiar with the endoscopic characteristics in order to diagnose and consider next steps appropriately.
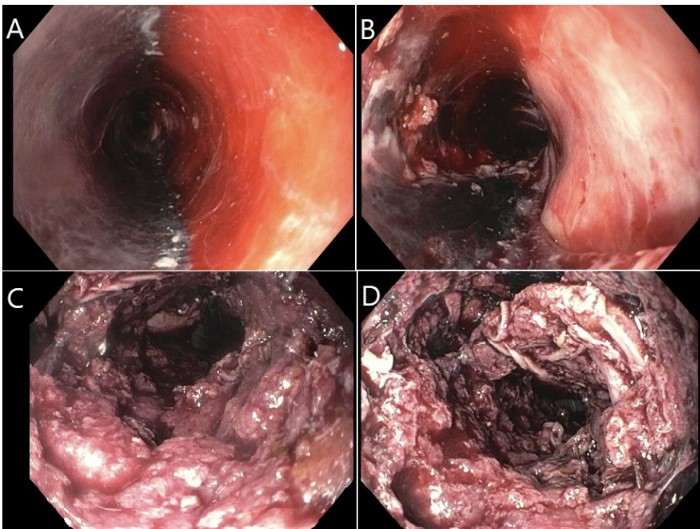
Figure: Figure 1. A. Necrosis and ischemia of the proximal esophagus. B: Necrosis and ischemia of the distal esophagus with mucosal sloughing. C and D: Extensive esophageal mucosal changes with active oozing of blood.
Disclosures:
Arvind Bussetty indicated no relevant financial relationships.
Toni Marie Chandler indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Arvind Bussetty, MD, Toni Marie Chandler, MD, Keerthana Kesavarapu, MD. P2306 - Endoscopic Findings of Necrotic Esophagus in the Setting of Suspected Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
