Monday Poster Session
Category: Esophagus
P2314 - Acute Dysphagia: A Rare Presentation of Graves’ Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KM
Karthik Mathialagan, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Karthik Mathialagan, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Prachi Pednekar, MD2
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Hospital, New Haven, CT
Introduction: Graves' disease is an autoimmune thyroid disorder that presents with a variety of extrathyroidal manifestations and the GI tract is a commonly affected extrathyroidal tissue. Dysphagia is usually a rare manifestation of hyperthyroidism and is described only in a few case reports. We describe a patient with Graves' disease who presented with dysphagia as the initial symptom.
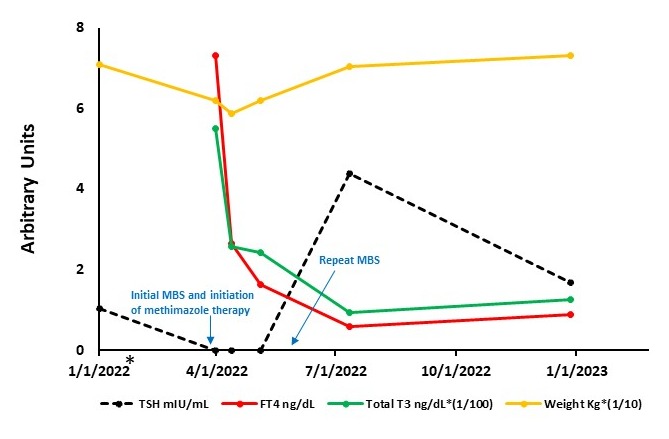
Case Description/Methods: A 44-year-old man with past medical history of prediabetes presented to the ER with new onset dysphagia, weight loss and dyspepsia for 6 weeks. He has had a choking sensation while swallowing solid food, along with a hacking cough, leading to a change to a liquid diet. Initial vitals were stable and the physical exam was unremarkable, without muscle weakness or abnormal reflexes. His labs showed normal CMP and CBC with low Thyroid Stimulating Hormone level (TSH) < 0.005 mIU/mL, elevated T3 of 549 ng/dL and free T4 of 7.3 ng/dL. Thyroglobulin antibody and thyrotropin receptor antibodies (TRAb) were elevated and Thyroid-stimulating immunoglobulin (TSI) was 471 % baseline (< 140% baseline). CT neck was unremarkable and thyroid ultrasound showed a diffusely enlarged, hypervascular thyroid without nodules. Modified Barium Swallow showed abnormal oral and pharyngeal swallow phase with increased residue. In the absence of other anatomic findings or explanations, a diagnosis of dysphagia secondary to Graves’ disease was made. He was started on methimazole and propranolol and in two months, his symptoms improved. His repeat blood work 6 months later showed TSH of 1.68 mIU/ml, normal free T4, T3, undetectable TSI, and TRAb.
Discussion: The major GI manifestations of Graves’ disease include increased appetite, achlorhydria, decreased GI transit time leading to increased frequency of bowel movements, impaired fat absorption causing steatorrhea and dyspepsia. Limited literature is present on the mechanism of esophageal or pharyngeal muscle involvement causing dysphagia. One proposed mechanism is the deposition of glycosaminoglycans leading to interstitial edema in the esophageal muscles and dysfunction. In a study of 30 patients with Graves’ disease, esophageal manometry showed the duration of contraction was significantly lower in hyperthyroid patients than in healthy controls. In conclusion, thyroid evaluation should be considered in the workup of patients presenting with dysphagia. Treatment with methimazole or propylthiouracil combined with a beta blocker has been shown to improve dysphagia in these patients.
Disclosures:
Karthik Mathialagan, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Prachi Pednekar, MD2. P2314 - Acute Dysphagia: A Rare Presentation of Graves’ Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Hospital, New Haven, CT
Introduction: Graves' disease is an autoimmune thyroid disorder that presents with a variety of extrathyroidal manifestations and the GI tract is a commonly affected extrathyroidal tissue. Dysphagia is usually a rare manifestation of hyperthyroidism and is described only in a few case reports. We describe a patient with Graves' disease who presented with dysphagia as the initial symptom.
Case Description/Methods: A 44-year-old man with past medical history of prediabetes presented to the ER with new onset dysphagia, weight loss and dyspepsia for 6 weeks. He has had a choking sensation while swallowing solid food, along with a hacking cough, leading to a change to a liquid diet. Initial vitals were stable and the physical exam was unremarkable, without muscle weakness or abnormal reflexes. His labs showed normal CMP and CBC with low Thyroid Stimulating Hormone level (TSH) < 0.005 mIU/mL, elevated T3 of 549 ng/dL and free T4 of 7.3 ng/dL. Thyroglobulin antibody and thyrotropin receptor antibodies (TRAb) were elevated and Thyroid-stimulating immunoglobulin (TSI) was 471 % baseline (< 140% baseline). CT neck was unremarkable and thyroid ultrasound showed a diffusely enlarged, hypervascular thyroid without nodules. Modified Barium Swallow showed abnormal oral and pharyngeal swallow phase with increased residue. In the absence of other anatomic findings or explanations, a diagnosis of dysphagia secondary to Graves’ disease was made. He was started on methimazole and propranolol and in two months, his symptoms improved. His repeat blood work 6 months later showed TSH of 1.68 mIU/ml, normal free T4, T3, undetectable TSI, and TRAb.
Discussion: The major GI manifestations of Graves’ disease include increased appetite, achlorhydria, decreased GI transit time leading to increased frequency of bowel movements, impaired fat absorption causing steatorrhea and dyspepsia. Limited literature is present on the mechanism of esophageal or pharyngeal muscle involvement causing dysphagia. One proposed mechanism is the deposition of glycosaminoglycans leading to interstitial edema in the esophageal muscles and dysfunction. In a study of 30 patients with Graves’ disease, esophageal manometry showed the duration of contraction was significantly lower in hyperthyroid patients than in healthy controls. In conclusion, thyroid evaluation should be considered in the workup of patients presenting with dysphagia. Treatment with methimazole or propylthiouracil combined with a beta blocker has been shown to improve dysphagia in these patients.
Figure: Changes in thyroid hormones, weight, and swallowing are shown over time. *The Baseline TSH was from 11/21/2018 but is indicated on the chart as 1/1/2022 for visual purposes. Text boxes indicate the time of methimazole initiation and swallowing studies. The X-axis has units adjusted for display on a single scale. T3 and weight were divided by 100 and 10, respectively, to match scaled unit ranges for TSH and free T4.
Abbreviations: TSH, thyroid stimulating hormone; FT4, free T4; MBS, modified barium swallow; Kg, kilogram
Abbreviations: TSH, thyroid stimulating hormone; FT4, free T4; MBS, modified barium swallow; Kg, kilogram
Disclosures:
Karthik Mathialagan indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Rofina Johnkennedy indicated no relevant financial relationships.
Prachi Pednekar indicated no relevant financial relationships.
Karthik Mathialagan, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Prachi Pednekar, MD2. P2314 - Acute Dysphagia: A Rare Presentation of Graves’ Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
