Monday Poster Session
Category: Esophagus
P2225 - Reducing Inappropriate Use of Proton Pump Inhibitors in Outpatient Settings: A Quality Improvement Project
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Saqr Alsakarneh, MD
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Saqr Alsakarneh, MD1, Vinay Jahagirdar, MD2, Noor Hassan, MD2, Ahmed Husain, MD3, Parth Sharma, MBBS4, Roshni Thomas, MD1, Zainab Humayan, MD1, Kevin Varghese, MD5, Julie Banderas, PharmD2, David Wooldridge, MD6
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City, Kansas City, MO; 4University of Missouri, Kansas City, MO; 5University of Missouri - Kansas City School of Medicine, Kansas City, KS; 6University of Missouri, Overland Park, KS
Introduction: Proton pump inhibitors (PPIs) are among the most commonly used medications worldwide. PPI overuse is not only linked to severe adverse effects like pneumonia and Clostridioides difficile infections, but also imposes economic costs and contributes to polypharmacy. The rate of inappropriately prescribed PPIs for patients at University Health (UH) internal medicine (IM) resident clinics between July and December 2023 was 66%. We aimed to reduce the rate of inappropriate PPI prescriptions among UH adult patients in resident clinics by 20% in three months.
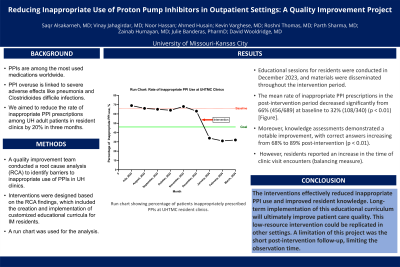
Methods: A quality improvement team conducted a root cause analysis (RCA) to identify barriers to inappropriate use of PPIs in UH clinics. Interventions were designed based on the RCA findings, which included the creation and implementation of customized educational curricula for IM residents. Educational efforts included in-person presentations and dissemination of infographics and handouts via email to IM residents. Additionally, pre- and post-intervention surveys were used to test the residents’ knowledge regarding the appropriate use of PPIs. The outcome measures were the percentage of patients inappropriately prescribed PPIs and resident knowledge of appropriate indications of PPIs. The interventions were complemented by Plan-Do-Study-Act (PDSA) cycles to ensure a comprehensive approach. A run chart was used for the analysis.
Results: Educational sessions for residents were conducted in December 2023, and materials were disseminated throughout the intervention period. The mean rate of inappropriate PPI prescriptions in the post-intervention period decreased significantly from 66% (456/689) at baseline to 32% (108/340) (p < 0.01) [Figure]. Moreover, knowledge assessments demonstrated a notable improvement, with correct answers increasing from 68% to 89% post-intervention (p < 0.01). However, residents reported an increase in the time of clinic visit encounters (balancing measure).
Discussion: The interventions effectively reduced inappropriate PPI use and improved resident knowledge. Long-term implementation of this educational curriculum will ultimately improve patient care quality. Plans for sustainability include integrating the educational curriculum into ongoing training and institutional practices. This low-resource intervention could be replicated in other settings. A limitation of this project was the short post-intervention follow-up, limiting the observation time.
Disclosures:
Saqr Alsakarneh, MD1, Vinay Jahagirdar, MD2, Noor Hassan, MD2, Ahmed Husain, MD3, Parth Sharma, MBBS4, Roshni Thomas, MD1, Zainab Humayan, MD1, Kevin Varghese, MD5, Julie Banderas, PharmD2, David Wooldridge, MD6. P2225 - Reducing Inappropriate Use of Proton Pump Inhibitors in Outpatient Settings: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City, Kansas City, MO; 4University of Missouri, Kansas City, MO; 5University of Missouri - Kansas City School of Medicine, Kansas City, KS; 6University of Missouri, Overland Park, KS
Introduction: Proton pump inhibitors (PPIs) are among the most commonly used medications worldwide. PPI overuse is not only linked to severe adverse effects like pneumonia and Clostridioides difficile infections, but also imposes economic costs and contributes to polypharmacy. The rate of inappropriately prescribed PPIs for patients at University Health (UH) internal medicine (IM) resident clinics between July and December 2023 was 66%. We aimed to reduce the rate of inappropriate PPI prescriptions among UH adult patients in resident clinics by 20% in three months.
Methods: A quality improvement team conducted a root cause analysis (RCA) to identify barriers to inappropriate use of PPIs in UH clinics. Interventions were designed based on the RCA findings, which included the creation and implementation of customized educational curricula for IM residents. Educational efforts included in-person presentations and dissemination of infographics and handouts via email to IM residents. Additionally, pre- and post-intervention surveys were used to test the residents’ knowledge regarding the appropriate use of PPIs. The outcome measures were the percentage of patients inappropriately prescribed PPIs and resident knowledge of appropriate indications of PPIs. The interventions were complemented by Plan-Do-Study-Act (PDSA) cycles to ensure a comprehensive approach. A run chart was used for the analysis.
Results: Educational sessions for residents were conducted in December 2023, and materials were disseminated throughout the intervention period. The mean rate of inappropriate PPI prescriptions in the post-intervention period decreased significantly from 66% (456/689) at baseline to 32% (108/340) (p < 0.01) [Figure]. Moreover, knowledge assessments demonstrated a notable improvement, with correct answers increasing from 68% to 89% post-intervention (p < 0.01). However, residents reported an increase in the time of clinic visit encounters (balancing measure).
Discussion: The interventions effectively reduced inappropriate PPI use and improved resident knowledge. Long-term implementation of this educational curriculum will ultimately improve patient care quality. Plans for sustainability include integrating the educational curriculum into ongoing training and institutional practices. This low-resource intervention could be replicated in other settings. A limitation of this project was the short post-intervention follow-up, limiting the observation time.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Ahmed Husain indicated no relevant financial relationships.
Parth Sharma indicated no relevant financial relationships.
Roshni Thomas indicated no relevant financial relationships.
Zainab Humayan indicated no relevant financial relationships.
Kevin Varghese indicated no relevant financial relationships.
Julie Banderas indicated no relevant financial relationships.
David Wooldridge indicated no relevant financial relationships.
Saqr Alsakarneh, MD1, Vinay Jahagirdar, MD2, Noor Hassan, MD2, Ahmed Husain, MD3, Parth Sharma, MBBS4, Roshni Thomas, MD1, Zainab Humayan, MD1, Kevin Varghese, MD5, Julie Banderas, PharmD2, David Wooldridge, MD6. P2225 - Reducing Inappropriate Use of Proton Pump Inhibitors in Outpatient Settings: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
