Monday Poster Session
Category: Esophagus
P2229 - Pathologic Evaluation to Determine Depth of Invasion Cutoff for Superficial Esophageal Submucosal Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Omar Saab, MD
Cleveland Clinic Foundation
Westlake, OH
Presenting Author(s)
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4
1Cleveland Clinic Foundation, Westlake, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: T1b esophageal adenocarcinoma (EAC) is at the intersection of endoscopic and surgical treatment. Superficial SM1, with low lymph node metastasis (LNM) risk, fits curative endoscopic resection criteria. SM2 and SM3 T1b tumors carry higher LNM risk, warranting surgical resection. Surgical specimens distinguish SM1, SM2, and SM3 by tumor depth into submucosa thirds. In endoscopic specimens, where whole submucosa isn't accessible to define SM1, a 500 micron invasion depth signifies superficial SM layer (first third). Origin of the 500 micron SM1 cut-off remains unclear. Our study aimed to establish the SM1 cut-off.
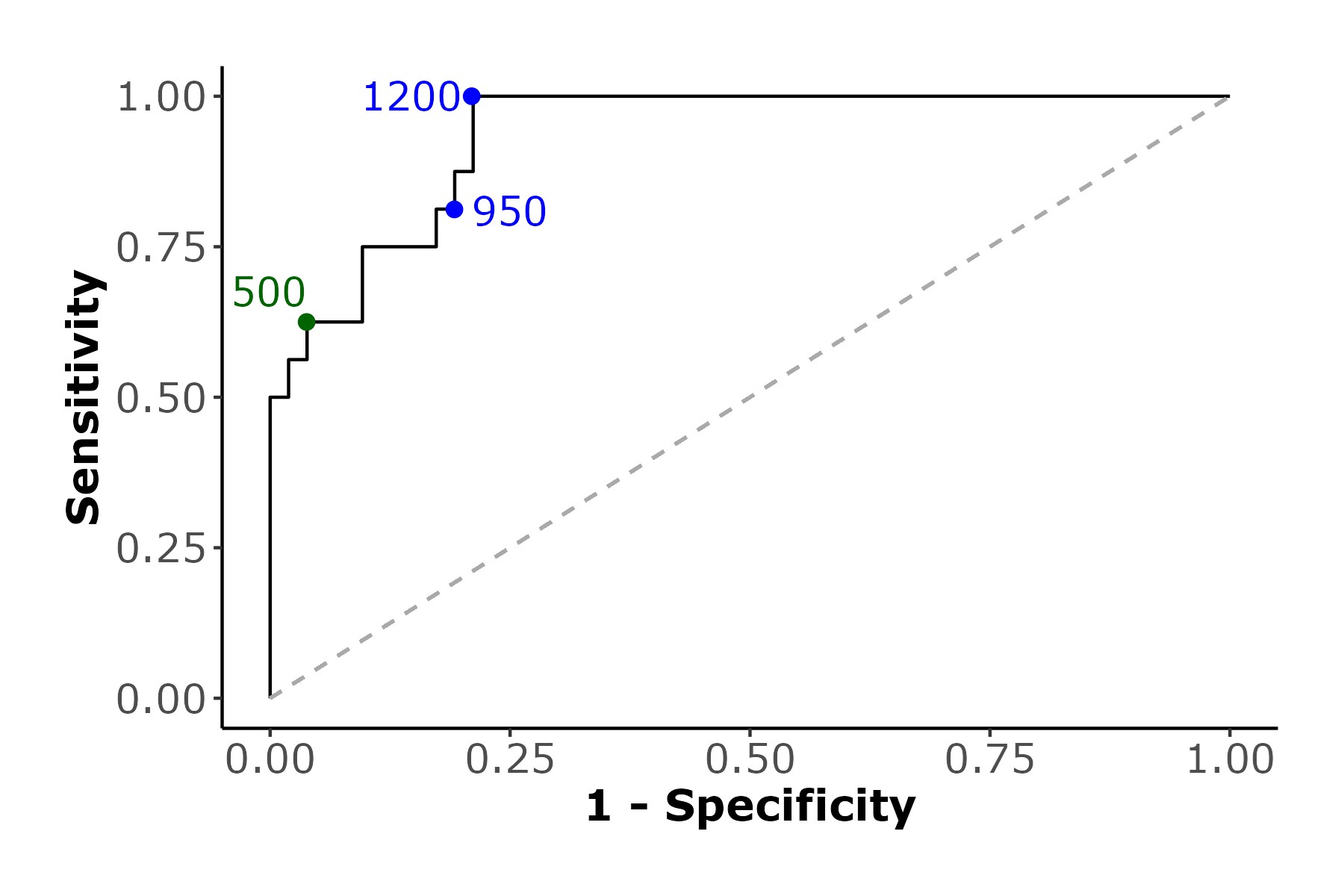
Methods: Retrospective cohort study of 120 patients who underwent esophagectomy for pathologically staged T1b EAC between 1988 and 2009, without prior chemotherapy or radiation. Pathologists measured exact submucosal invasion depth in microns and percentage of submucosal involvement. Fisher’s exact test assessed the association between depths less than 500 microns and tumors within SM1. Receiver operating characteristic (ROC) curve analysis evaluated sensitivity, specificity, and predictive values across various cutoffs predicting invasion within SM1. The study calculated the area under the ROC curve (AUC) and diagnostic measures for different cutoffs, including 500 microns, plotted on an ROC curve. Optimal cutoffs were determined based on Youden’s index, proximity to the optimal cutoff (1,0) on the ROC plot, and balancing sensitivity and specificity.
Results: In 120 T1b EAC patients undergoing esophagectomy alone, 68 with pathologic samples were analyzed. The optimal cut-off determined by Youden’s index near (0,1) on the curve was 1200 microns. At this threshold, sensitivity was 100%, indicating all SM1 depths in our cohort were ≤1200 microns. Specificity was 78.8%, meaning 78.8% of tumors invading beyond SM1 exceeded 1200 microns. The balance point for sensitivity and specificity was at 950 microns. Using 500 microns yielded lower sensitivity (62.5%) but higher specificity (96.2%). The model's AUC was 0.94, showing a 94% probability that a randomly selected person with SM1 depth ≤1200 microns had greater depth compared to one with depth beyond SM1.
Discussion: For T1b EAC our study suggests that 950 microns would be the optimal cut-off for superficial submucosal EAC, rather than the 500 microns that is currently used. Extending the micron cut-off for superficial submucosal SM1 EAC could allow more patients to avoid unnecessary surgery.
Disclosures:
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4. P2229 - Pathologic Evaluation to Determine Depth of Invasion Cutoff for Superficial Esophageal Submucosal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Westlake, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: T1b esophageal adenocarcinoma (EAC) is at the intersection of endoscopic and surgical treatment. Superficial SM1, with low lymph node metastasis (LNM) risk, fits curative endoscopic resection criteria. SM2 and SM3 T1b tumors carry higher LNM risk, warranting surgical resection. Surgical specimens distinguish SM1, SM2, and SM3 by tumor depth into submucosa thirds. In endoscopic specimens, where whole submucosa isn't accessible to define SM1, a 500 micron invasion depth signifies superficial SM layer (first third). Origin of the 500 micron SM1 cut-off remains unclear. Our study aimed to establish the SM1 cut-off.
Methods: Retrospective cohort study of 120 patients who underwent esophagectomy for pathologically staged T1b EAC between 1988 and 2009, without prior chemotherapy or radiation. Pathologists measured exact submucosal invasion depth in microns and percentage of submucosal involvement. Fisher’s exact test assessed the association between depths less than 500 microns and tumors within SM1. Receiver operating characteristic (ROC) curve analysis evaluated sensitivity, specificity, and predictive values across various cutoffs predicting invasion within SM1. The study calculated the area under the ROC curve (AUC) and diagnostic measures for different cutoffs, including 500 microns, plotted on an ROC curve. Optimal cutoffs were determined based on Youden’s index, proximity to the optimal cutoff (1,0) on the ROC plot, and balancing sensitivity and specificity.
Results: In 120 T1b EAC patients undergoing esophagectomy alone, 68 with pathologic samples were analyzed. The optimal cut-off determined by Youden’s index near (0,1) on the curve was 1200 microns. At this threshold, sensitivity was 100%, indicating all SM1 depths in our cohort were ≤1200 microns. Specificity was 78.8%, meaning 78.8% of tumors invading beyond SM1 exceeded 1200 microns. The balance point for sensitivity and specificity was at 950 microns. Using 500 microns yielded lower sensitivity (62.5%) but higher specificity (96.2%). The model's AUC was 0.94, showing a 94% probability that a randomly selected person with SM1 depth ≤1200 microns had greater depth compared to one with depth beyond SM1.
Discussion: For T1b EAC our study suggests that 950 microns would be the optimal cut-off for superficial submucosal EAC, rather than the 500 microns that is currently used. Extending the micron cut-off for superficial submucosal SM1 EAC could allow more patients to avoid unnecessary surgery.
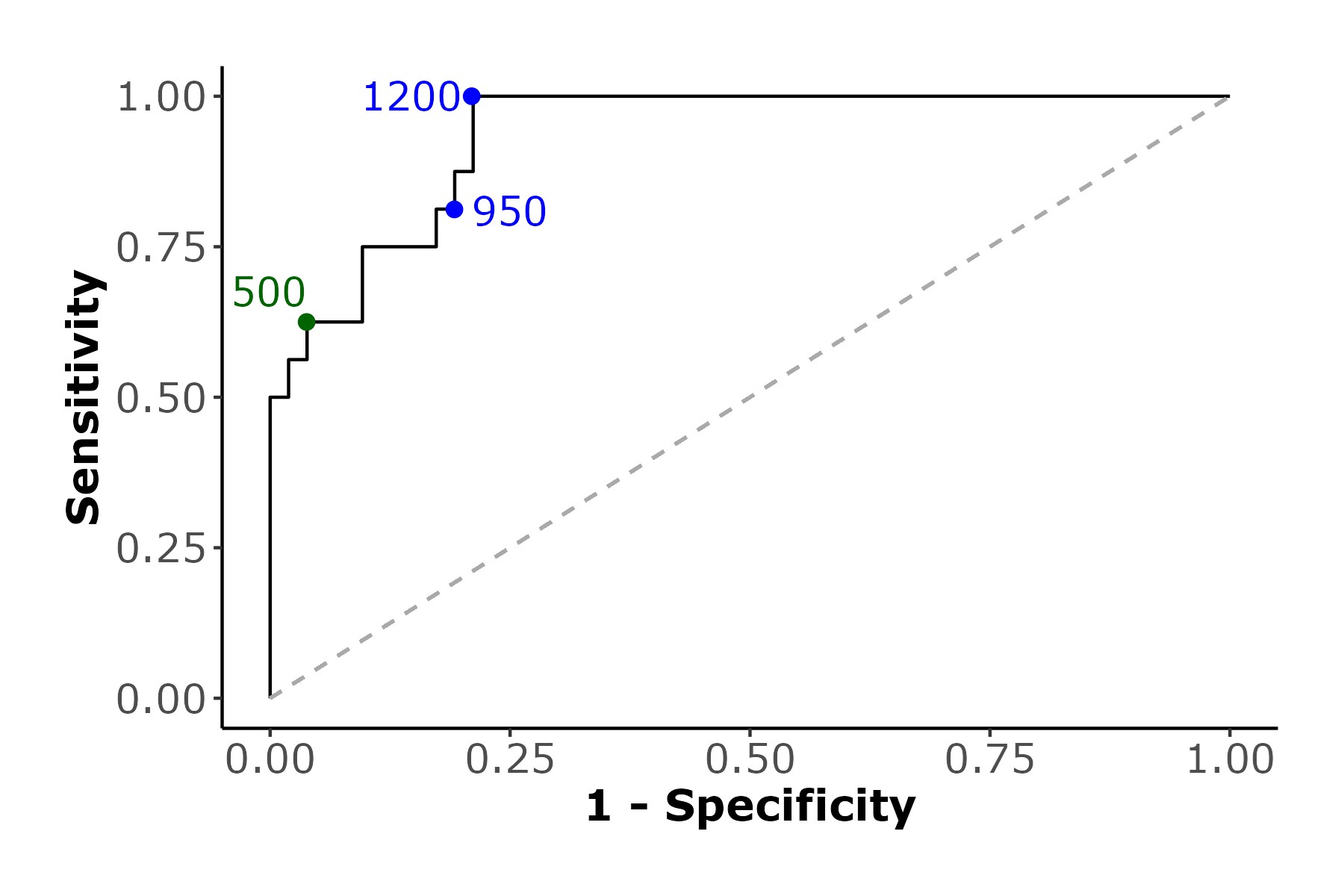
Figure: Figure 1. ROC Curve of Depth of the tumor in microns versus the tumor being within the SM1.
Disclosures:
Omar Saab indicated no relevant financial relationships.
Xuefeng Zhang indicated no relevant financial relationships.
James Bena indicated no relevant financial relationships.
Siva Raja indicated no relevant financial relationships.
Amit Bhatt indicated no relevant financial relationships.
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4. P2229 - Pathologic Evaluation to Determine Depth of Invasion Cutoff for Superficial Esophageal Submucosal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
