Monday Poster Session
Category: Esophagus
P2239 - Uncommon Presentation of Esophageal Foreign Body Impaction in an Elderly Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Amil Shah, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Amil Shah, DO, Uday Patel, DO, Bryant Javier, DO, Meghan Timmerman, DO
Parkview Medical Center, Pueblo, CO
Introduction: Foreign body impaction in the esophagus among adults is uncommon and presents with dysphagia, odynophagia, chest pain, or respiratory distress. Diagnosis is made by history, prompt evaluation by endoscopic examination, or thorough radiographic examination if not directly visualized. Removal of the foreign body, either surgically or endoscopically, is crucial to prevent life-threatening complications including esophageal perforation, fistula, mediastinitis, and airway obstruction.
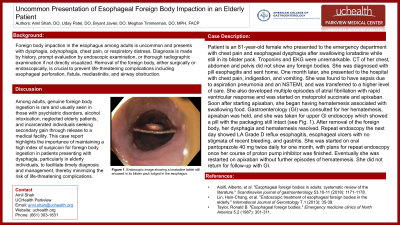
Case Description/Methods: Patient is an 81-year-old female who presented to the emergency department with chest pain and esophageal dysphagia after swallowing loratadine while still in its blister pack. Troponins and EKG were unremarkable. CT of her chest, abdomen and pelvis did not show any foreign bodies. She was diagnosed with pill esophagitis and sent home. One month later, she presented to the hospital with chest pain, indigestion, and vomiting. She was found to have sepsis due to aspiration pneumonia and an NSTEMI, and was transferred to a higher level of care. She also developed multiple episodes of atrial fibrillation with rapid ventricular response and was started on metoprolol succinate and apixaban. Soon after starting apixaban, she began having hematemesis associated with swallowing food. Gastroenterology (GI) was consulted for her hematemesis, apixaban was held, and she was taken for upper GI endoscopy which showed a pill with the packaging still intact. After removal of the foreign body, her dysphagia and hematemesis resolved. Repeat endoscopy the next day showed LA Grade D reflux esophagitis, esophageal ulcers with no stigmata of recent bleeding, and gastritis. She was started on oral pantoprazole 40 mg twice daily for one month, with plans for repeat endoscopy once her course of proton pump inhibitor was finished. Eventually she was restarted on apixaban without further episodes of hematemesis. She did not return for follow-up with GI.
Discussion: Among adults, genuine foreign body ingestion is rare and usually seen in those with psychiatric disorders, alcohol intoxication, neglected elderly patients, and incarcerated individuals seeking secondary gain through release to a medical facility. This case report highlights the importance of maintaining a high index of suspicion for foreign body ingestion in patients presenting with dysphagia, particularly in elderly individuals, to facilitate timely diagnosis and management, thereby minimizing the risk of life-threatening complications.
Disclosures:
Amil Shah, DO, Uday Patel, DO, Bryant Javier, DO, Meghan Timmerman, DO. P2239 - Uncommon Presentation of Esophageal Foreign Body Impaction in an Elderly Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Parkview Medical Center, Pueblo, CO
Introduction: Foreign body impaction in the esophagus among adults is uncommon and presents with dysphagia, odynophagia, chest pain, or respiratory distress. Diagnosis is made by history, prompt evaluation by endoscopic examination, or thorough radiographic examination if not directly visualized. Removal of the foreign body, either surgically or endoscopically, is crucial to prevent life-threatening complications including esophageal perforation, fistula, mediastinitis, and airway obstruction.
Case Description/Methods: Patient is an 81-year-old female who presented to the emergency department with chest pain and esophageal dysphagia after swallowing loratadine while still in its blister pack. Troponins and EKG were unremarkable. CT of her chest, abdomen and pelvis did not show any foreign bodies. She was diagnosed with pill esophagitis and sent home. One month later, she presented to the hospital with chest pain, indigestion, and vomiting. She was found to have sepsis due to aspiration pneumonia and an NSTEMI, and was transferred to a higher level of care. She also developed multiple episodes of atrial fibrillation with rapid ventricular response and was started on metoprolol succinate and apixaban. Soon after starting apixaban, she began having hematemesis associated with swallowing food. Gastroenterology (GI) was consulted for her hematemesis, apixaban was held, and she was taken for upper GI endoscopy which showed a pill with the packaging still intact. After removal of the foreign body, her dysphagia and hematemesis resolved. Repeat endoscopy the next day showed LA Grade D reflux esophagitis, esophageal ulcers with no stigmata of recent bleeding, and gastritis. She was started on oral pantoprazole 40 mg twice daily for one month, with plans for repeat endoscopy once her course of proton pump inhibitor was finished. Eventually she was restarted on apixaban without further episodes of hematemesis. She did not return for follow-up with GI.
Discussion: Among adults, genuine foreign body ingestion is rare and usually seen in those with psychiatric disorders, alcohol intoxication, neglected elderly patients, and incarcerated individuals seeking secondary gain through release to a medical facility. This case report highlights the importance of maintaining a high index of suspicion for foreign body ingestion in patients presenting with dysphagia, particularly in elderly individuals, to facilitate timely diagnosis and management, thereby minimizing the risk of life-threatening complications.
Disclosures:
Amil Shah indicated no relevant financial relationships.
Uday Patel indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Meghan Timmerman indicated no relevant financial relationships.
Amil Shah, DO, Uday Patel, DO, Bryant Javier, DO, Meghan Timmerman, DO. P2239 - Uncommon Presentation of Esophageal Foreign Body Impaction in an Elderly Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
