Monday Poster Session
Category: Esophagus
P2243 - Beyond the Food Bolus: Esophageal Perforation After Rigid Esophagoscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Danzhu Zhao, DO
University of Connecticut Health Center
WEST HARTFORD, CT
Presenting Author(s)
Danzhu Zhao, DO1, Minh Thu T.. Nguyen, MD1, Bianca Thakkar, DO1, Lisa Rossi, MD2
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health Center, Hartford, CT
Introduction: Esophageal food bolus impactions (EFBI) frequently prompt GI consultations. Although endoscopic removal succeeds in most cases, prolonged EFBI can lead to rare yet serious complications like esophageal perforation.
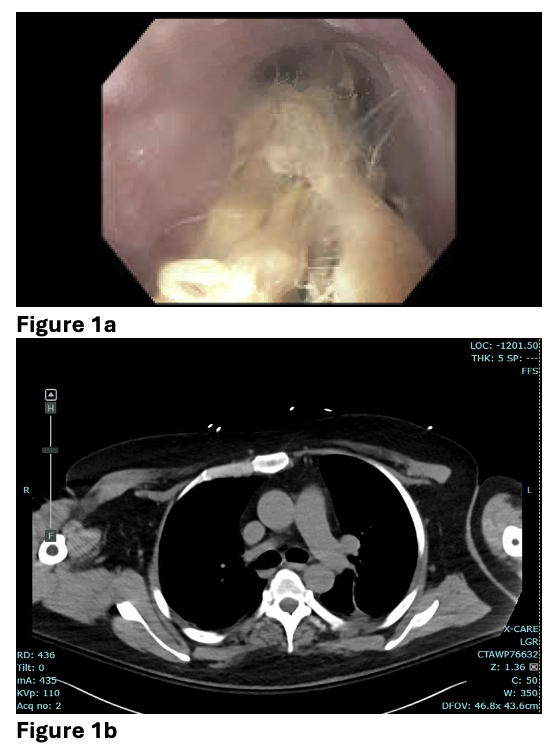
Case Description/Methods: A 53-year-old man with muscular dystrophy, asthma, and seasonal allergies presented to the ED unable to swallow after eating pulled pork three days prior. Flexible esophagogastroduodenoscopy (EGD) that evening showed a ringed esophagus with linear furrows, but the food bolus could not be fully removed after three hours of attempts, so the procedure was stopped without biopsy (Fig. 1a). A subsequent chest CT scan showed no perforation at that time (Fig. 1b).
General surgery performed rigid esophagoscopy, finding an impacted, macerated food bolus without a stricture. It was removed with forceps at 25-30 cm with minimal resistance noted at 40 cm, and the scope passed into the stomach. Subsequent flexible EGD revealed a full-thickness perforation 4 cm proximal to the gastroesophageal junction, possibly due to necrosis from the earlier procedure. A left thoracostomy tube was inserted, and the pleura over the esophagus was incised, followed by suturing. The patient was successfully extubated but required a PEG tube due to oropharyngeal dysphagia.
Discussion: Esophageal perforation is a rare but serious risk during endoscopic removal of EFBI. Before attempting removal, conservative measures such as glucagon, benzodiazepines, calcium channel blockers, nitrates, and physical maneuvers may be considered. If unsuccessful, flexible EGD is performed with intubation to protect the airway and allow for extended procedure times. Should flexible endoscopy prove ineffective, the subsequent step typically involves rigid esophagoscopy performed by surgeons.
Our patient, possibly with eosinophilic esophagitis (EoE), based on typical EGD findings and a history of allergy and asthma, faces higher perforation risks due to inflamed, scarred esophagi typical of EoE. However, EoE diagnosis remains unconfirmed without biopsies. Concurrent esophageal dysmotility, linked to his muscular dystrophy, may contribute to food impaction and warrants further investigation via esophageal manometry. This case highlights the importance of understanding the potential complications if EFBI removal fails and the subsequent steps, particularly in a hospital setting prepared for emergent surgical repair after perforation.
Disclosures:
Danzhu Zhao, DO1, Minh Thu T.. Nguyen, MD1, Bianca Thakkar, DO1, Lisa Rossi, MD2. P2243 - Beyond the Food Bolus: Esophageal Perforation After Rigid Esophagoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health Center, Hartford, CT
Introduction: Esophageal food bolus impactions (EFBI) frequently prompt GI consultations. Although endoscopic removal succeeds in most cases, prolonged EFBI can lead to rare yet serious complications like esophageal perforation.
Case Description/Methods: A 53-year-old man with muscular dystrophy, asthma, and seasonal allergies presented to the ED unable to swallow after eating pulled pork three days prior. Flexible esophagogastroduodenoscopy (EGD) that evening showed a ringed esophagus with linear furrows, but the food bolus could not be fully removed after three hours of attempts, so the procedure was stopped without biopsy (Fig. 1a). A subsequent chest CT scan showed no perforation at that time (Fig. 1b).
General surgery performed rigid esophagoscopy, finding an impacted, macerated food bolus without a stricture. It was removed with forceps at 25-30 cm with minimal resistance noted at 40 cm, and the scope passed into the stomach. Subsequent flexible EGD revealed a full-thickness perforation 4 cm proximal to the gastroesophageal junction, possibly due to necrosis from the earlier procedure. A left thoracostomy tube was inserted, and the pleura over the esophagus was incised, followed by suturing. The patient was successfully extubated but required a PEG tube due to oropharyngeal dysphagia.
Discussion: Esophageal perforation is a rare but serious risk during endoscopic removal of EFBI. Before attempting removal, conservative measures such as glucagon, benzodiazepines, calcium channel blockers, nitrates, and physical maneuvers may be considered. If unsuccessful, flexible EGD is performed with intubation to protect the airway and allow for extended procedure times. Should flexible endoscopy prove ineffective, the subsequent step typically involves rigid esophagoscopy performed by surgeons.
Our patient, possibly with eosinophilic esophagitis (EoE), based on typical EGD findings and a history of allergy and asthma, faces higher perforation risks due to inflamed, scarred esophagi typical of EoE. However, EoE diagnosis remains unconfirmed without biopsies. Concurrent esophageal dysmotility, linked to his muscular dystrophy, may contribute to food impaction and warrants further investigation via esophageal manometry. This case highlights the importance of understanding the potential complications if EFBI removal fails and the subsequent steps, particularly in a hospital setting prepared for emergent surgical repair after perforation.
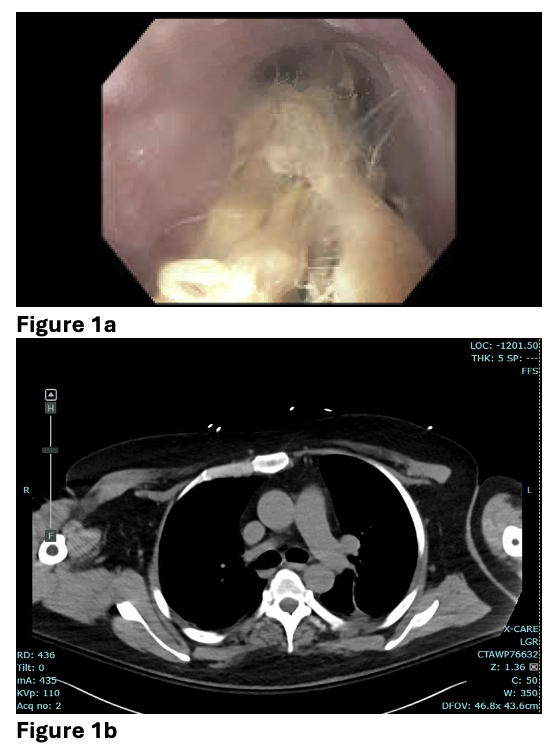
Figure: Figure 1a. Food was found in the middle and lower third of the esophagus, with esophageal mucosal changes suspicious for eosinophilic esophagitis.
Figure 1b. CT chest showed no evidence of esophageal perforation following initial flexible EGD.
Figure 1b. CT chest showed no evidence of esophageal perforation following initial flexible EGD.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Lisa Rossi indicated no relevant financial relationships.
Danzhu Zhao, DO1, Minh Thu T.. Nguyen, MD1, Bianca Thakkar, DO1, Lisa Rossi, MD2. P2243 - Beyond the Food Bolus: Esophageal Perforation After Rigid Esophagoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
