Monday Poster Session
Category: Colorectal Cancer Prevention
P2152 - Colorectal Carcinoma Screening: Addressing Language Barriers in a Community-Based Clinic
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- TN
Tripti Nagar, MD
Wayne State University School of Medicine
Rochester, MI
Presenting Author(s)
Tripti Nagar, MD1, Jai Kumar, MD2, Wadid Sirry, MD1
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Troy, MI
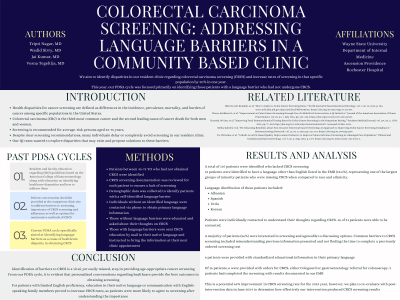
Introduction: Healthcare disparities for cancer screening are differences in the incidence, prevalence, mortality, and cancer burden among specific populations. Differences in the quality of health are most prominently seen in and across racial, ethnic, and socioeconomic groups. Understanding population-specific differences are imperative in improving patient health outcomes and access to treatment. Despite clear guidelines for colorectal cancer screening (CRCS), many individuals delay or avoid screening in our resident clinic. This project aims to identify disparities in regarding CRCS and increase CRCS rates by 20% in one year. This PDSA cycle was focused on identifying patients with limited English proficiency (LEP).
Methods: Patients aged 45-75 without CRCS were identified. Those who were lost to follow up, refused demographic questioning of race, gender, ethnicity or primary language were excluded. Patients with and without LEP were contacted by phone and asked about their thoughts on CRCS. Those with self-identified LEP were sent CRCS education in their native language by mail and were instructed to bring the information at their next visit.
Results: Pre-intervention, 107 patients lacked CRCS. 21 patients (19.6%) were identified to have a language other than English listed in the EMR, representing one of the largest minority groups who were missing CRCS when compared to racial, ethnic and gender-based disparities evaluated in prior PDSA cycles. Language distribution included Albanian, Spanish, Urdu and Korean. 16 of 21 patients were individually contacted and 56% of patients were interested in CRCS screening. 37.5% of patients were agreeable for Cologaurd or gastroenterology referral orders for colonoscopy. 50% of these patients completed screening by the start of the post-intervention window.
Discussion: Our study has a potential 46% improvement for CRCS for 2024. A formal post-intervention analysis is planned in June 2024. The most important takeaway from this study is identifying barriers to care in CRCS is a vital and easily missed step in providing age-appropriate screening. Our PDSA cycle makes it evident that personalized conversations with patients provide the best outcomes for preventative health care. For patients with LEP, education in their native language or presence of an English-speaking family member is likely to increase screening rates as patients are more likely to understand the risk of waiting and the benefits of screening.
Disclosures:
Tripti Nagar, MD1, Jai Kumar, MD2, Wadid Sirry, MD1. P2152 - Colorectal Carcinoma Screening: Addressing Language Barriers in a Community-Based Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Troy, MI
Introduction: Healthcare disparities for cancer screening are differences in the incidence, prevalence, mortality, and cancer burden among specific populations. Differences in the quality of health are most prominently seen in and across racial, ethnic, and socioeconomic groups. Understanding population-specific differences are imperative in improving patient health outcomes and access to treatment. Despite clear guidelines for colorectal cancer screening (CRCS), many individuals delay or avoid screening in our resident clinic. This project aims to identify disparities in regarding CRCS and increase CRCS rates by 20% in one year. This PDSA cycle was focused on identifying patients with limited English proficiency (LEP).
Methods: Patients aged 45-75 without CRCS were identified. Those who were lost to follow up, refused demographic questioning of race, gender, ethnicity or primary language were excluded. Patients with and without LEP were contacted by phone and asked about their thoughts on CRCS. Those with self-identified LEP were sent CRCS education in their native language by mail and were instructed to bring the information at their next visit.
Results: Pre-intervention, 107 patients lacked CRCS. 21 patients (19.6%) were identified to have a language other than English listed in the EMR, representing one of the largest minority groups who were missing CRCS when compared to racial, ethnic and gender-based disparities evaluated in prior PDSA cycles. Language distribution included Albanian, Spanish, Urdu and Korean. 16 of 21 patients were individually contacted and 56% of patients were interested in CRCS screening. 37.5% of patients were agreeable for Cologaurd or gastroenterology referral orders for colonoscopy. 50% of these patients completed screening by the start of the post-intervention window.
Discussion: Our study has a potential 46% improvement for CRCS for 2024. A formal post-intervention analysis is planned in June 2024. The most important takeaway from this study is identifying barriers to care in CRCS is a vital and easily missed step in providing age-appropriate screening. Our PDSA cycle makes it evident that personalized conversations with patients provide the best outcomes for preventative health care. For patients with LEP, education in their native language or presence of an English-speaking family member is likely to increase screening rates as patients are more likely to understand the risk of waiting and the benefits of screening.
Disclosures:
Tripti Nagar indicated no relevant financial relationships.
Jai Kumar indicated no relevant financial relationships.
Wadid Sirry indicated no relevant financial relationships.
Tripti Nagar, MD1, Jai Kumar, MD2, Wadid Sirry, MD1. P2152 - Colorectal Carcinoma Screening: Addressing Language Barriers in a Community-Based Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
