Monday Poster Session
Category: Colorectal Cancer Prevention
P2154 - Strategies and Outcomes for Improving Bowel Preparation for Colonoscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anna Goebel, MD
University of Pennsylvania Health System
Philadelphia, PA
Presenting Author(s)
Anna Goebel, MD1, Sarjukumar Panchal, MD, PharmD2, Alexandra C. Leto, MD2, Farees Saqlain, MD1, Liza Hillel, CPNP3, Shivan Mehta, MD2, Shazia M. Siddique, MD, MSHP2
1University of Pennsylvania Health System, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Penn Medicine, Philadlephia, PA
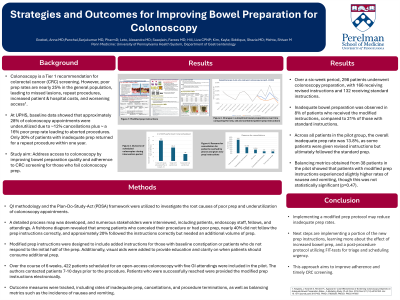
Introduction: Colonoscopy is a tier 1 recommendation for colorectal cancer (CRC) screening, but poor bowel prep leads to missed lesions, repeat procedures, and poor resource utilization. Within the general population, rates of inadequate prep are estimated to be as high as 25%. Quality data from an outpatient endoscopy center within the University of Pennsylvania Health System (UPHS)showed approximately 16% of patients who undergo colonoscopy have inadequate prep. While patients are recommended to repeat colonoscopy at the next available appointment, only 30% had a repeat colonoscopy within a year. This study aimed to address access to colonoscopy by improving bowel preparation and adherence to CRC screening for those who fail colonoscopy prep.
Methods: The Plan-Do-Study-Act framework was used. Process mapping from scheduling to procedure completion was assessed. Incorrect prep initiation and insufficient 2L of PEG were identified as key issues, comprising 60% of root causes. Patient factors included pre-existing constipation,high-risk medication use, and health literacy. Revised prep instructions were created to a) increase Miralax dose if non-response to initial half of split-dose prep, b) more clearly delineate medication cessation protocols, and c) enhance visual instructions. Instructions were delivered in electronic format 7-10 days before the procedure date to patients reached via phone. Outcome measures included rates of inadequate prep, cancellations, procedure terminations, and balancing metrics of nausea and vomiting incidence.
Results: Over six weeks, 298 patients underwent colonoscopy prep, with 166 receiving revised instructions and 132 receiving standard instructions. Inadequate prep was observed in 8% of patients who received modified instructions compared to 21% with standard instructions. Amongst all patients in the pilot group, the inadequate prep rate was 13.8%, given some patients were called with the revised prep, but ultimately followed standard prep. Balancing metrics obtained from 38 patients in the pilot, showed patients with modified prep instructions experienced slightly higher rates of nausea and vomiting (p=0.47).
Discussion: Implementing a modified prep protocol may reduce inadequate prep rates.Next steps are implementing a portion of the new prep instructions, learning more about the effect of increased bowel prep, and a post-procedure protocol utilizing FIT-tests for triage and scheduling urgency. This approach aims to improve adherence and timely CRC screening.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anna Goebel, MD1, Sarjukumar Panchal, MD, PharmD2, Alexandra C. Leto, MD2, Farees Saqlain, MD1, Liza Hillel, CPNP3, Shivan Mehta, MD2, Shazia M. Siddique, MD, MSHP2. P2154 - Strategies and Outcomes for Improving Bowel Preparation for Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania Health System, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Penn Medicine, Philadlephia, PA
Introduction: Colonoscopy is a tier 1 recommendation for colorectal cancer (CRC) screening, but poor bowel prep leads to missed lesions, repeat procedures, and poor resource utilization. Within the general population, rates of inadequate prep are estimated to be as high as 25%. Quality data from an outpatient endoscopy center within the University of Pennsylvania Health System (UPHS)showed approximately 16% of patients who undergo colonoscopy have inadequate prep. While patients are recommended to repeat colonoscopy at the next available appointment, only 30% had a repeat colonoscopy within a year. This study aimed to address access to colonoscopy by improving bowel preparation and adherence to CRC screening for those who fail colonoscopy prep.
Methods: The Plan-Do-Study-Act framework was used. Process mapping from scheduling to procedure completion was assessed. Incorrect prep initiation and insufficient 2L of PEG were identified as key issues, comprising 60% of root causes. Patient factors included pre-existing constipation,high-risk medication use, and health literacy. Revised prep instructions were created to a) increase Miralax dose if non-response to initial half of split-dose prep, b) more clearly delineate medication cessation protocols, and c) enhance visual instructions. Instructions were delivered in electronic format 7-10 days before the procedure date to patients reached via phone. Outcome measures included rates of inadequate prep, cancellations, procedure terminations, and balancing metrics of nausea and vomiting incidence.
Results: Over six weeks, 298 patients underwent colonoscopy prep, with 166 receiving revised instructions and 132 receiving standard instructions. Inadequate prep was observed in 8% of patients who received modified instructions compared to 21% with standard instructions. Amongst all patients in the pilot group, the inadequate prep rate was 13.8%, given some patients were called with the revised prep, but ultimately followed standard prep. Balancing metrics obtained from 38 patients in the pilot, showed patients with modified prep instructions experienced slightly higher rates of nausea and vomiting (p=0.47).
Discussion: Implementing a modified prep protocol may reduce inadequate prep rates.Next steps are implementing a portion of the new prep instructions, learning more about the effect of increased bowel prep, and a post-procedure protocol utilizing FIT-tests for triage and scheduling urgency. This approach aims to improve adherence and timely CRC screening.

Figure: Comparing suboptimal prep in patients who underwent colonoscopy using new versus old perp
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anna Goebel indicated no relevant financial relationships.
Sarjukumar Panchal indicated no relevant financial relationships.
Alexandra Leto indicated no relevant financial relationships.
Farees Saqlain indicated no relevant financial relationships.
Liza Hillel: AbbVie – Speakers Bureau.
Shivan Mehta: Guardant Health – Advisory Committee/Board Member.
Shazia Siddique indicated no relevant financial relationships.
Anna Goebel, MD1, Sarjukumar Panchal, MD, PharmD2, Alexandra C. Leto, MD2, Farees Saqlain, MD1, Liza Hillel, CPNP3, Shivan Mehta, MD2, Shazia M. Siddique, MD, MSHP2. P2154 - Strategies and Outcomes for Improving Bowel Preparation for Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
