Monday Poster Session
Category: Colon
P2061 - Constipation Catastrophe: Unraveling the Mystery of Megacolon and Achalasia in a Young Girl
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Parul Berry, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Parul Berry, MBBS1, Umang Arora, MBBS, MD2, Madhusudhan KS, MD2, Prasenjit Das, MD2, Nihar Ranjan Dash, MBBS, MS2, Sahil Khanna, MBBS, MS1, Govind Makharia, MD, DM2
1Mayo Clinic, Rochester, MN; 2All India Institute of Medical Sciences, New Delhi, Delhi, India
Introduction: Idiopathic slow-transit constipation poses significant diagnostic and therapeutic challenges due to limited insight into it’s pathogenesis. We present a case of an 18-year-old female who presented with megacolon requiring emergent colectomy and was diagnosed concomitantly with Achalasia cardia.
Case Description/Methods: An 18-year-old female presented with chronic constipation for 6 years, characterized by infrequent, hard stools every 2-3 days, eventually becoming less frequent despite the use of laxatives and enemas.
At presentation, she had not passed stools for 3 months and developed progressive abdominal distension with dull, aching pain. Her condition was complicated by a weight loss of 15 kg, although she did not report dysphagia.On examination, she was emaciated and examination revealed multiple hard lumps in the upper abdomen with diffuse tenderness.
During her hospital stay. She developed worsening abdominal pain and tenderness necessitating an emergency laparotomy with a suspicion of bowel ischemia. Intra-operatively, a massively dilated colon with impacted fecoliths from the sigmoid colon to the cecum, along with a papery thin colon with areas of gangrenous changes and impending perforation, was discovered.A subtotal colectomy with removal of impacted fecoliths and end-ileostomy was performed.
Histopathological examination of the resected specimen revealed marked asymmetrical hypertrophy of muscularis propria without vacuolations or inclusions, and CD117 immunostaining indicated a loss of interstitial cells of Cajal. The final histopathological diagnosis was Idiopathic segmental muscular hypertrophy with partial desmopathy and mesenchymopathy along with ischemic infarct. Post-operatively, the patient recovered well with regular stomal passage of fecal content 4 times/day. Esophageal manometry was performed on follow-up which indicated absence of peristalsis with a high integrated relaxation pressure of 20.2mm Hg consistent with type I achalasia cardia. Timed barium swallow showed the classical rat-tail appearance seen in achalasia. Genetic evaluation for the association is awaited.
Discussion: This case underscores a complex presentation of pan-gastrointestinal (GI) motility disorder, including megacolon and achalasia type I, associated with abnormal inner circular muscular layer of the colonic wall and loss of interstitial cells of Cajal. There is need for further research into the genetic and biological underpinnings of visceral myopathy and multifocal motility disorders.
Disclosures:
Parul Berry, MBBS1, Umang Arora, MBBS, MD2, Madhusudhan KS, MD2, Prasenjit Das, MD2, Nihar Ranjan Dash, MBBS, MS2, Sahil Khanna, MBBS, MS1, Govind Makharia, MD, DM2. P2061 - Constipation Catastrophe: Unraveling the Mystery of Megacolon and Achalasia in a Young Girl, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2All India Institute of Medical Sciences, New Delhi, Delhi, India
Introduction: Idiopathic slow-transit constipation poses significant diagnostic and therapeutic challenges due to limited insight into it’s pathogenesis. We present a case of an 18-year-old female who presented with megacolon requiring emergent colectomy and was diagnosed concomitantly with Achalasia cardia.
Case Description/Methods: An 18-year-old female presented with chronic constipation for 6 years, characterized by infrequent, hard stools every 2-3 days, eventually becoming less frequent despite the use of laxatives and enemas.
At presentation, she had not passed stools for 3 months and developed progressive abdominal distension with dull, aching pain. Her condition was complicated by a weight loss of 15 kg, although she did not report dysphagia.On examination, she was emaciated and examination revealed multiple hard lumps in the upper abdomen with diffuse tenderness.
During her hospital stay. She developed worsening abdominal pain and tenderness necessitating an emergency laparotomy with a suspicion of bowel ischemia. Intra-operatively, a massively dilated colon with impacted fecoliths from the sigmoid colon to the cecum, along with a papery thin colon with areas of gangrenous changes and impending perforation, was discovered.A subtotal colectomy with removal of impacted fecoliths and end-ileostomy was performed.
Histopathological examination of the resected specimen revealed marked asymmetrical hypertrophy of muscularis propria without vacuolations or inclusions, and CD117 immunostaining indicated a loss of interstitial cells of Cajal. The final histopathological diagnosis was Idiopathic segmental muscular hypertrophy with partial desmopathy and mesenchymopathy along with ischemic infarct. Post-operatively, the patient recovered well with regular stomal passage of fecal content 4 times/day. Esophageal manometry was performed on follow-up which indicated absence of peristalsis with a high integrated relaxation pressure of 20.2mm Hg consistent with type I achalasia cardia. Timed barium swallow showed the classical rat-tail appearance seen in achalasia. Genetic evaluation for the association is awaited.
Discussion: This case underscores a complex presentation of pan-gastrointestinal (GI) motility disorder, including megacolon and achalasia type I, associated with abnormal inner circular muscular layer of the colonic wall and loss of interstitial cells of Cajal. There is need for further research into the genetic and biological underpinnings of visceral myopathy and multifocal motility disorders.
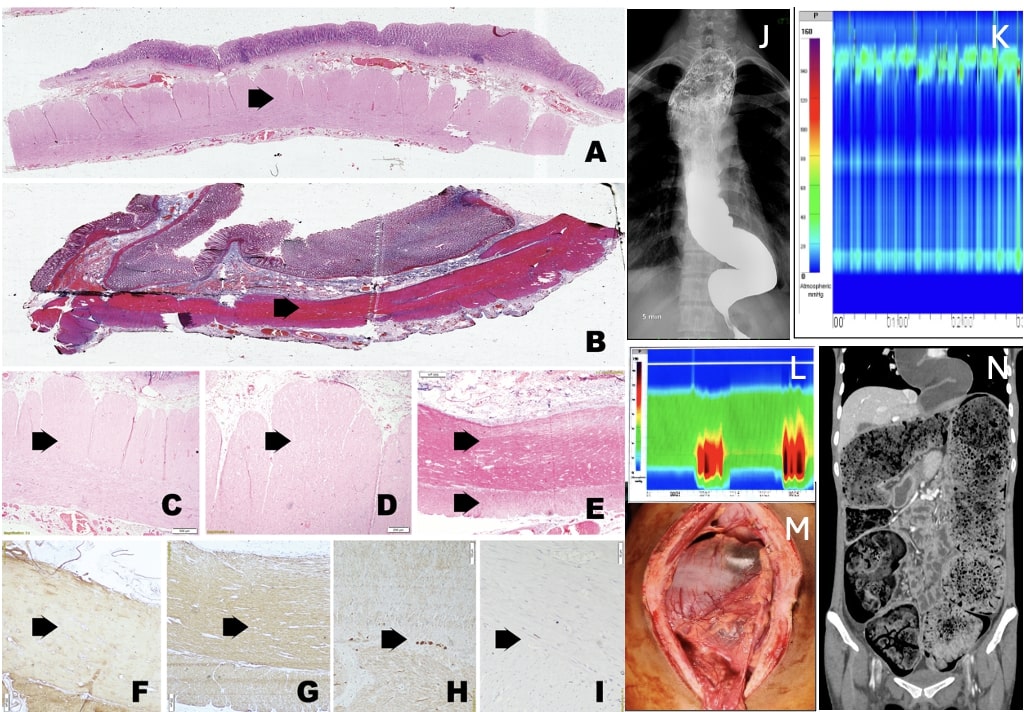
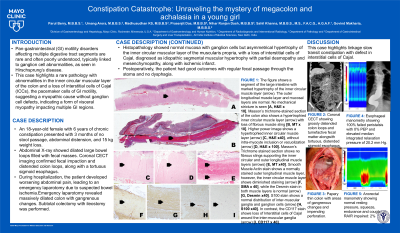
Figure: A: A segment of the large intestine with marked hypertrophy of the inner circular muscle layer (arrow). The outer longitudinal muscle layer and mucosal layers are normal. No mechanical stricture is seen.
B: Masson’s trichrome-stained section of the colon shows a hypertrophied inner circular muscle layer (arrow) with loss of fibrous muscle sling
C: Higher power image shows a hypertrophied inner circular muscle layer (arrow)
D: Higher power image shows a hypertrophied inner circular muscle layer (arrow)
without intra-myocyte inclusion or vacuolization (arrow)
E: Masson’s Trichrome stained section shows no fibrous slings supporting the inner circular and outer longitudinal muscle layers (arrows)
F: Smooth Muscle Actin stain shows a normally stained outer longitudinal muscle layer, however, the inner circular muscle layer shows diminished staining (arrow)
G: Smooth Muscle Actin stain shows a normally stained outer longitudinal muscle layer, however, the inner circular muscle layer shows diminished staining (arrow) while the Desmin stain in both muscle layers is normal (arrow)
H: S100 stain shows a normal distribution of inter-muscular ganglia and ganglion cells (arrow)
I: the CD117 stain shows loss of Interstitial cells of Cajal around the inter-muscular ganglia (arrow)
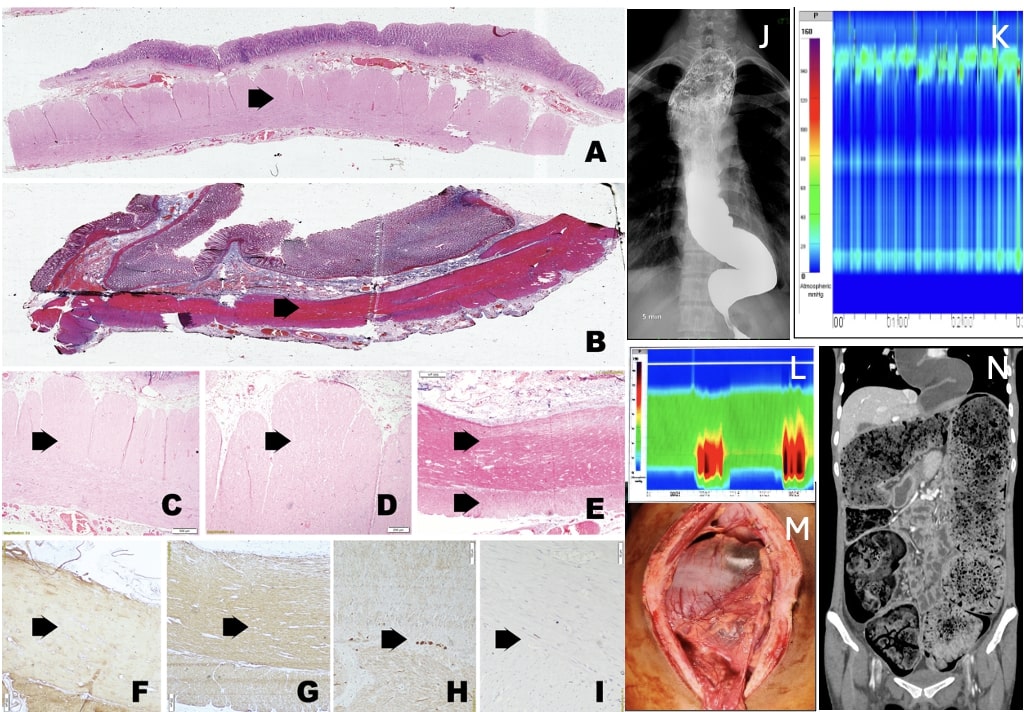
J and K: Esophageal manometry showing 100% failed peristalsis with 0% PEP and elevated median integrated relaxation pressure of 20.2 mm Hg
L: Anorectal manometry showing normal resting pressure, squeeze, endurance and cough RAIR impaired:2%
M: Papery thin colon with areas of gangrenous changes and impending perforation
N: Coronal CECT showing grossly distended colon loops and tumefactive fecal matter alongwith tortuous, distended sigmoid esophagus
B: Masson’s trichrome-stained section of the colon shows a hypertrophied inner circular muscle layer (arrow) with loss of fibrous muscle sling
C: Higher power image shows a hypertrophied inner circular muscle layer (arrow)
D: Higher power image shows a hypertrophied inner circular muscle layer (arrow)
without intra-myocyte inclusion or vacuolization (arrow)
E: Masson’s Trichrome stained section shows no fibrous slings supporting the inner circular and outer longitudinal muscle layers (arrows)
F: Smooth Muscle Actin stain shows a normally stained outer longitudinal muscle layer, however, the inner circular muscle layer shows diminished staining (arrow)
G: Smooth Muscle Actin stain shows a normally stained outer longitudinal muscle layer, however, the inner circular muscle layer shows diminished staining (arrow) while the Desmin stain in both muscle layers is normal (arrow)
H: S100 stain shows a normal distribution of inter-muscular ganglia and ganglion cells (arrow)
I: the CD117 stain shows loss of Interstitial cells of Cajal around the inter-muscular ganglia (arrow)
J and K: Esophageal manometry showing 100% failed peristalsis with 0% PEP and elevated median integrated relaxation pressure of 20.2 mm Hg
L: Anorectal manometry showing normal resting pressure, squeeze, endurance and cough RAIR impaired:2%
M: Papery thin colon with areas of gangrenous changes and impending perforation
N: Coronal CECT showing grossly distended colon loops and tumefactive fecal matter alongwith tortuous, distended sigmoid esophagus
Disclosures:
Parul Berry indicated no relevant financial relationships.
Umang Arora indicated no relevant financial relationships.
Madhusudhan KS indicated no relevant financial relationships.
Prasenjit Das indicated no relevant financial relationships.
Nihar Ranjan Dash indicated no relevant financial relationships.
Sahil Khanna: Ferring Pharmaceuticals, Inc. – Grant/Research Support. Finch – Grant/Research Support. Pfizer – Grant/Research Support. Probio Tech, LLC – Consultant. Rise – Consultant. Seres Therapeutics – Grant/Research Support. Takeda – Consultant. Vedanta – Grant/Research Support.
Govind Makharia indicated no relevant financial relationships.
Parul Berry, MBBS1, Umang Arora, MBBS, MD2, Madhusudhan KS, MD2, Prasenjit Das, MD2, Nihar Ranjan Dash, MBBS, MS2, Sahil Khanna, MBBS, MS1, Govind Makharia, MD, DM2. P2061 - Constipation Catastrophe: Unraveling the Mystery of Megacolon and Achalasia in a Young Girl, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
