Monday Poster Session
Category: Colon
P2016 - Drug-Induced Colitis Secondary to Dasatinib Therapy in a Patient With Established Ulcerative Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Raza Muhammad, DO
University of Chicago Northshore
Chicago, IL
Presenting Author(s)
Raza Muhammad, DO1, Maryam Haider, MD2, Samuel Engman, DO1, Omar Abdelsadek, MD3, Joel Retsky, MD4
1University of Chicago Northshore, Evanston, IL; 2University of Chicago Endeavor Health, Evanston, IL; 3NorthShore University HealthSystem, Chicago, IL; 4University of Chicago Pritzker School of Medicine, NorthShore University Medical Group, Highland Park, IL
Introduction: Dasatinib is a tyrosine kinase inhibitor and first-line treatment for chronic myelogenous leukemia(CML). Dasatinib therapy has known side effects including myelosuppression, anemia, hemorrhage, and pleural effusion. Some gastrointestinal side effects such as diarrhea and abdominal pain have been documented. There have been cases of dasatinib-induced colitis, however this is an uncommon occurrence. We present a rare presentation of Dasatinib-induced colitis in a patient with already established ulcerative colitis(UC).
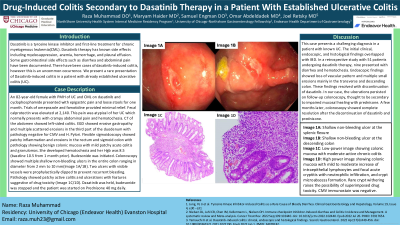
Case Description/Methods: An 82-year-old female with PMH of UC and CML on dasatinib and cyclophosphamide presented with epigastric pain and loose stools for one month. Trials of omeprazole and famotidine provided minimal relief. Fecal calprotectin was elevated at 2,140. This pain was atypical of her UC which normally presents with crampy abdominal pain and hematochezia. CT of theabdomen showed left-sided colitis. EGD showed erosive gastropathy and multiple scattered erosions in the third part of the duodenum with pathology negative for CMV and H. Pylori. Flexible sigmoidoscopy showed patchy inflammation and erosions in the rectum and sigmoid colon with pathology showing benign colonic mucosa with mild patchy acute colitis and granulomas. Budesonide was initiated, however, she was readmitted with hematochezia and Hgb of 8.5(baseline 10.5,1 month prior). Colonoscopy showed multiple shallow non-bleeding ulcers in the entire colon ranging in diameter from 2 mm to 10 mm(Image 1A/1B). Two ulcers with visible vessels were prophylactically clipped to prevent recurrent bleeding. Pathology showed patchy active colitis and ulcerations with features suggestive of drug toxicity (Image 2A/2B).Dasatinib was held, budesonide was stopped and the patient was started on Prednisone 40 mg daily.
Discussion: This case presents a challenging diagnosis in a patient with known UC. The initial clinical, endoscopic, and histological findings overlapped with IBD. In a retrospective study with 51 patients undergoing dasatinib therapy, nine presented with diarrhea and hematochezia. Endoscopic findings showed loss of vascular pattern and multiple small erosions mainly in the transverse and descending colon. These findings were resolved with discontinuation of dasatinib. In our case, the ulcerations persisted on follow-up colonoscopy, thought to be secondary to impaired mucosal healing with prednisone. A few months later, colonoscopy showed complete resolution after the discontinuation of dasatinib and prednisone.

Disclosures:
Raza Muhammad, DO1, Maryam Haider, MD2, Samuel Engman, DO1, Omar Abdelsadek, MD3, Joel Retsky, MD4. P2016 - Drug-Induced Colitis Secondary to Dasatinib Therapy in a Patient With Established Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago Northshore, Evanston, IL; 2University of Chicago Endeavor Health, Evanston, IL; 3NorthShore University HealthSystem, Chicago, IL; 4University of Chicago Pritzker School of Medicine, NorthShore University Medical Group, Highland Park, IL
Introduction: Dasatinib is a tyrosine kinase inhibitor and first-line treatment for chronic myelogenous leukemia(CML). Dasatinib therapy has known side effects including myelosuppression, anemia, hemorrhage, and pleural effusion. Some gastrointestinal side effects such as diarrhea and abdominal pain have been documented. There have been cases of dasatinib-induced colitis, however this is an uncommon occurrence. We present a rare presentation of Dasatinib-induced colitis in a patient with already established ulcerative colitis(UC).
Case Description/Methods: An 82-year-old female with PMH of UC and CML on dasatinib and cyclophosphamide presented with epigastric pain and loose stools for one month. Trials of omeprazole and famotidine provided minimal relief. Fecal calprotectin was elevated at 2,140. This pain was atypical of her UC which normally presents with crampy abdominal pain and hematochezia. CT of theabdomen showed left-sided colitis. EGD showed erosive gastropathy and multiple scattered erosions in the third part of the duodenum with pathology negative for CMV and H. Pylori. Flexible sigmoidoscopy showed patchy inflammation and erosions in the rectum and sigmoid colon with pathology showing benign colonic mucosa with mild patchy acute colitis and granulomas. Budesonide was initiated, however, she was readmitted with hematochezia and Hgb of 8.5(baseline 10.5,1 month prior). Colonoscopy showed multiple shallow non-bleeding ulcers in the entire colon ranging in diameter from 2 mm to 10 mm(Image 1A/1B). Two ulcers with visible vessels were prophylactically clipped to prevent recurrent bleeding. Pathology showed patchy active colitis and ulcerations with features suggestive of drug toxicity (Image 2A/2B).Dasatinib was held, budesonide was stopped and the patient was started on Prednisone 40 mg daily.
Discussion: This case presents a challenging diagnosis in a patient with known UC. The initial clinical, endoscopic, and histological findings overlapped with IBD. In a retrospective study with 51 patients undergoing dasatinib therapy, nine presented with diarrhea and hematochezia. Endoscopic findings showed loss of vascular pattern and multiple small erosions mainly in the transverse and descending colon. These findings were resolved with discontinuation of dasatinib. In our case, the ulcerations persisted on follow-up colonoscopy, thought to be secondary to impaired mucosal healing with prednisone. A few months later, colonoscopy showed complete resolution after the discontinuation of dasatinib and prednisone.

Figure: Image 1A: Shallow non-bleeding ulcer at the splenic flexure
Image 1B: Shallow non-bleeding ulcer at the descending colon
Image 2A: Low-power image showing colonic mucosa with moderate active chronic colitis
Image 2B: High power image showing colonic mucosa with mild to moderate increase of intraepithelial lymphocytes and focal acute cryptitis with neutrophilic infiltration, and crypt microabscess formation. Rare crypt withering raises the possibility of superimposed drug toxicity. CMV immunostain was negative.
Image 1B: Shallow non-bleeding ulcer at the descending colon
Image 2A: Low-power image showing colonic mucosa with moderate active chronic colitis
Image 2B: High power image showing colonic mucosa with mild to moderate increase of intraepithelial lymphocytes and focal acute cryptitis with neutrophilic infiltration, and crypt microabscess formation. Rare crypt withering raises the possibility of superimposed drug toxicity. CMV immunostain was negative.
Disclosures:
Raza Muhammad indicated no relevant financial relationships.
Maryam Haider indicated no relevant financial relationships.
Samuel Engman indicated no relevant financial relationships.
Omar Abdelsadek indicated no relevant financial relationships.
Joel Retsky indicated no relevant financial relationships.
Raza Muhammad, DO1, Maryam Haider, MD2, Samuel Engman, DO1, Omar Abdelsadek, MD3, Joel Retsky, MD4. P2016 - Drug-Induced Colitis Secondary to Dasatinib Therapy in a Patient With Established Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
