Monday Poster Session
Category: Colon
P2021 - PCR Positive with Toxin Negative Stool and Underlying Severe Clostridioides difficile Infection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Jennifer Ma, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Jennifer Ma, MD1, Kevin K. Yu, MD1, Mason Motakef, BS1, Mohammad Asim Amjad, MD2, Brooks D. Cash, MD, FACG3, Gautam Sikka, MD4
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health Science Center, Houston, TX; 3McGovern Medical School at UTHealth, Houston, TX; 4University of Texas, Houston, TX
Introduction: Current ACG guidelines for Clostridioides difficile (CDI) testing comprises of stool sampling for PCR and toxin detection. A positive PCR result indicates either colonization or infection and should prompt confirmatory testing. However, such testing may result in PCR+/toxin- results even when there is a strong suspicion for CDI. Here, we identify a case of PCR+/toxin- severe CDI necessitating escalation of therapy.
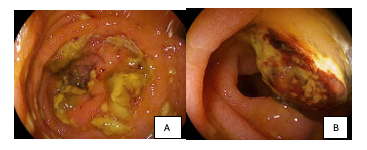
Case Description/Methods: A 66-year-old female with a history of HTN and chronic anemia on HCTZ and bisoprolol presented with fatigue, nausea, diarrhea, and vomiting for one month. She was admitted with a Hgb of 4.7 g/dL, acute renal failure (BUN 145 mg/dL / Cr16 mg/dL) and hyperkalemia (K 6.3 mEq/L). She received emergent dialysis and 2u RBC. Renal failure workup demonstrated +ANA 1:1280 speckled, +U1snRNP, low C3, MPO+, cANCA+, and pauci-immune glomerulonephritis on biopsy. Her course was complicated by persistent leukocytosis and respiratory failure. Because of her clinical worsening, even though her stool was PCR+/toxin- for CDI, oral vancomycin 125 mg q6H was initiated. She was also treated for a UTI with cefepime and meropenem for pneumonia, but her clinical status worsened. Corticosteroids and anticoagulation were desired for suspected autoimmune vasculitis, but she developed hematochezia and worsening anemia. Colonoscopy revealed diffuse pseudomembranous colitis with colonic and rectal ulcerations. CDI therapy was escalated with the addition of metronidazole 500 mg q8H for severe CDI. After clinical improvement, she was transitioned to fidaxomicin 200 mg q12H and her vasculitis-induced respiratory failure improved with steroids and anticoagulation permitting extubation. She was eventually discharged to home on room air.
Discussion: This case highlights the need to keep CDI in the differential of patients who are immunocompromised, even in the scenario of PCR+/toxin- stool testing. If endoscopic appearance is classic and histology confirms active CDI, we recommend treatment regardless of confirmatory CDI testing results.
Disclosures:
Jennifer Ma, MD1, Kevin K. Yu, MD1, Mason Motakef, BS1, Mohammad Asim Amjad, MD2, Brooks D. Cash, MD, FACG3, Gautam Sikka, MD4. P2021 - PCR Positive with Toxin Negative Stool and Underlying Severe <i>Clostridioides difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health Science Center, Houston, TX; 3McGovern Medical School at UTHealth, Houston, TX; 4University of Texas, Houston, TX
Introduction: Current ACG guidelines for Clostridioides difficile (CDI) testing comprises of stool sampling for PCR and toxin detection. A positive PCR result indicates either colonization or infection and should prompt confirmatory testing. However, such testing may result in PCR+/toxin- results even when there is a strong suspicion for CDI. Here, we identify a case of PCR+/toxin- severe CDI necessitating escalation of therapy.
Case Description/Methods: A 66-year-old female with a history of HTN and chronic anemia on HCTZ and bisoprolol presented with fatigue, nausea, diarrhea, and vomiting for one month. She was admitted with a Hgb of 4.7 g/dL, acute renal failure (BUN 145 mg/dL / Cr16 mg/dL) and hyperkalemia (K 6.3 mEq/L). She received emergent dialysis and 2u RBC. Renal failure workup demonstrated +ANA 1:1280 speckled, +U1snRNP, low C3, MPO+, cANCA+, and pauci-immune glomerulonephritis on biopsy. Her course was complicated by persistent leukocytosis and respiratory failure. Because of her clinical worsening, even though her stool was PCR+/toxin- for CDI, oral vancomycin 125 mg q6H was initiated. She was also treated for a UTI with cefepime and meropenem for pneumonia, but her clinical status worsened. Corticosteroids and anticoagulation were desired for suspected autoimmune vasculitis, but she developed hematochezia and worsening anemia. Colonoscopy revealed diffuse pseudomembranous colitis with colonic and rectal ulcerations. CDI therapy was escalated with the addition of metronidazole 500 mg q8H for severe CDI. After clinical improvement, she was transitioned to fidaxomicin 200 mg q12H and her vasculitis-induced respiratory failure improved with steroids and anticoagulation permitting extubation. She was eventually discharged to home on room air.
Discussion: This case highlights the need to keep CDI in the differential of patients who are immunocompromised, even in the scenario of PCR+/toxin- stool testing. If endoscopic appearance is classic and histology confirms active CDI, we recommend treatment regardless of confirmatory CDI testing results.
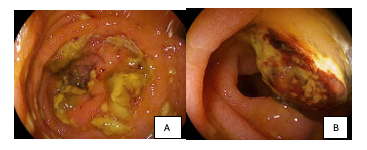
Figure: A. Pseudomembranous Colitis
B. Sigmoid Ulcer
B. Sigmoid Ulcer
Disclosures:
Jennifer Ma indicated no relevant financial relationships.
Kevin Yu indicated no relevant financial relationships.
Mason Motakef indicated no relevant financial relationships.
Mohammad Asim Amjad indicated no relevant financial relationships.
Brooks Cash: Abbvie – Consultant, Speakers Bureau. Alnylam – Speakers Bureau. Ardelyx – Consultant, Speakers Bureau. Astra Zeneca – Consultant, Speakers Bureau. Phathom – Consultant, Speakers Bureau. QOL – Speakers Bureau. Salix – Speakers Bureau. Vibrant Advisory Board – Advisory Committee/Board Member.
Gautam Sikka indicated no relevant financial relationships.
Jennifer Ma, MD1, Kevin K. Yu, MD1, Mason Motakef, BS1, Mohammad Asim Amjad, MD2, Brooks D. Cash, MD, FACG3, Gautam Sikka, MD4. P2021 - PCR Positive with Toxin Negative Stool and Underlying Severe <i>Clostridioides difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
