Monday Poster Session
Category: Colon
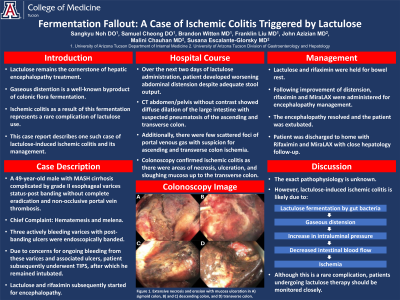
P2022 - Fermentation Fallout: A Case of Ischemic Colitis Triggered by Lactulose
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Samuel H. Cheong, DO
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Sangkyu Noh, DO1, Samuel H. Cheong, DO1, Brandon Witten, MD2, Franklin Liu, MD1, John Azizian, MD1, Malini Chauhan, MD1, Susana Escalante-Glorsky, MD1
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ
Introduction: Lactulose remains the cornerstone of hepatic encephalopathy treatment, and gaseous distention is a well-known byproduct of colonic flora fermentation. Ischemic colitis as a result of this fermentation represents a rare complication of lactulose use with only sporadic accounts of this phenomenon in the literature. In this case report, we describe one such case of lactulose-induced ischemic colitis and its subsequent management.
Case Description/Methods: A 49-year-old male with NASH cirrhosis complicated by grade II esophageal varices status-post banding without complete eradication and nonocclusive portal vein thrombosis presented with hematemesis and melena. Three actively bleeding varices with post-banding ulcers were endoscopically banded. Due to concerns for ongoing bleeding from these varices/associated ulcers, the patient subsequently underwent TIPS, after which he remained intubated. Lactulose and rifaximin were subsequently started for encephalopathy.
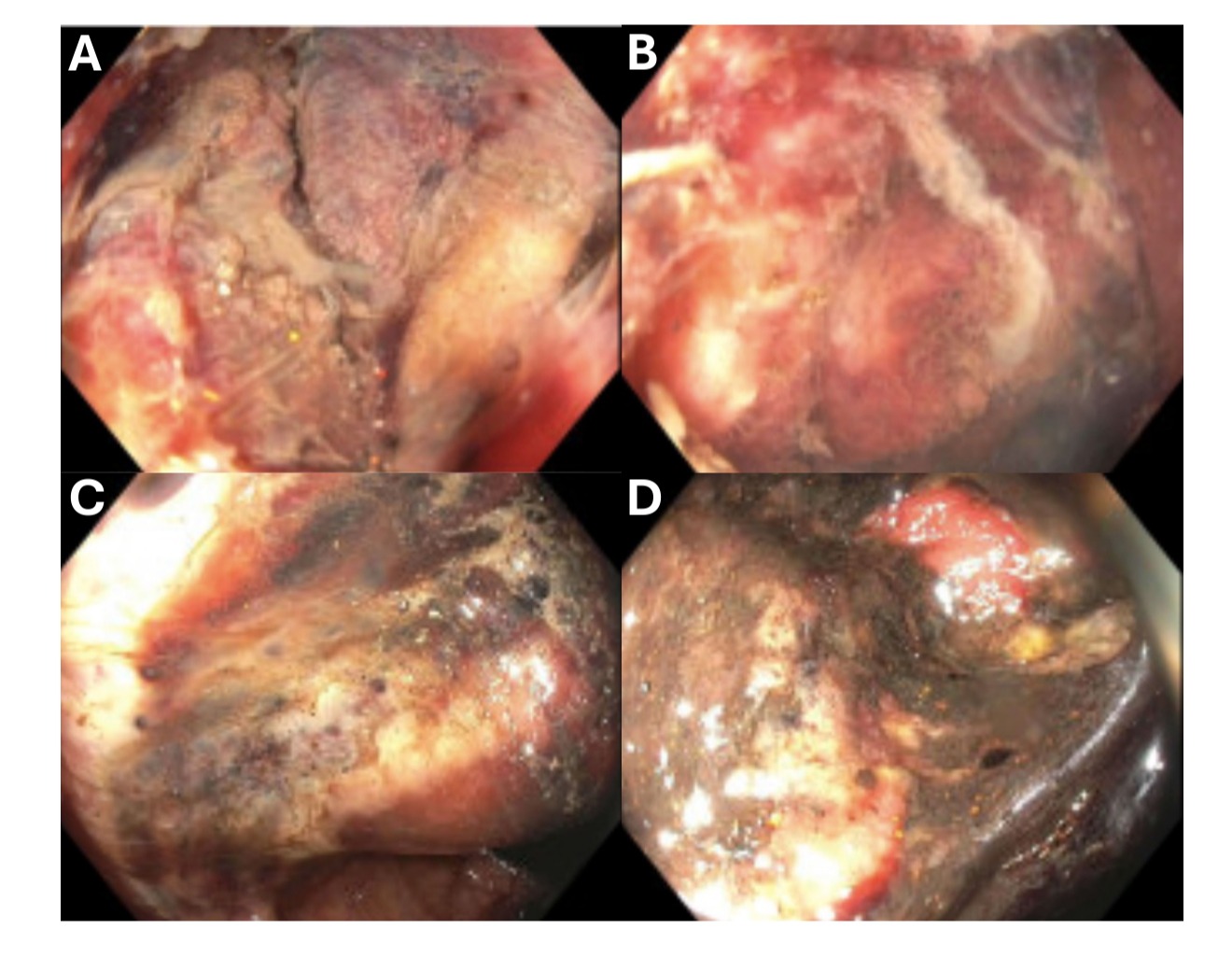
Over the next two days of lactulose administration, he developed worsening abdominal distention despite adequate stool output. CT abdomen/pelvis without contrast showed diffuse dilation of the large intestine with suspected pneumatosis of the ascending and transverse colon. Additionally, there were few scattered foci of portal venous gas with suspicion for ascending and transverse colon ischemia. Colonoscopy confirmed ischemic colitis as there were areas of necrosis, ulcerations, and sloughing mucosa up to the transverse colon, which was the furthest point traversed. Lactulose and rifaximin were then held for bowel rest. Following improvement of distention on KUB, rifaximin and MiraLAX were administered for encephalopathy management in anticipation of extubation. The encephalopathy resolved, and the patient was extubated and eventually discharged home with rifaximin and MiraLAX with close hepatology follow-up.
Discussion: While the exact pathophysiology is unknown, lactulose-associated ischemic colitis is likely due to lactulose fermentation by gut bacteria leading to gaseous distention and subsequent increase in intraluminal pressure causing decreased intestinal blood flow and ischemia. Although this is a rare complication, patients undergoing lactulose therapy should be monitored closely, with signs of intestinal ischemia prompting further investigation as well as potentially holding lactulose to promote bowel rest.
Disclosures:
Sangkyu Noh, DO1, Samuel H. Cheong, DO1, Brandon Witten, MD2, Franklin Liu, MD1, John Azizian, MD1, Malini Chauhan, MD1, Susana Escalante-Glorsky, MD1. P2022 - Fermentation Fallout: A Case of Ischemic Colitis Triggered by Lactulose, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ
Introduction: Lactulose remains the cornerstone of hepatic encephalopathy treatment, and gaseous distention is a well-known byproduct of colonic flora fermentation. Ischemic colitis as a result of this fermentation represents a rare complication of lactulose use with only sporadic accounts of this phenomenon in the literature. In this case report, we describe one such case of lactulose-induced ischemic colitis and its subsequent management.
Case Description/Methods: A 49-year-old male with NASH cirrhosis complicated by grade II esophageal varices status-post banding without complete eradication and nonocclusive portal vein thrombosis presented with hematemesis and melena. Three actively bleeding varices with post-banding ulcers were endoscopically banded. Due to concerns for ongoing bleeding from these varices/associated ulcers, the patient subsequently underwent TIPS, after which he remained intubated. Lactulose and rifaximin were subsequently started for encephalopathy.
Over the next two days of lactulose administration, he developed worsening abdominal distention despite adequate stool output. CT abdomen/pelvis without contrast showed diffuse dilation of the large intestine with suspected pneumatosis of the ascending and transverse colon. Additionally, there were few scattered foci of portal venous gas with suspicion for ascending and transverse colon ischemia. Colonoscopy confirmed ischemic colitis as there were areas of necrosis, ulcerations, and sloughing mucosa up to the transverse colon, which was the furthest point traversed. Lactulose and rifaximin were then held for bowel rest. Following improvement of distention on KUB, rifaximin and MiraLAX were administered for encephalopathy management in anticipation of extubation. The encephalopathy resolved, and the patient was extubated and eventually discharged home with rifaximin and MiraLAX with close hepatology follow-up.
Discussion: While the exact pathophysiology is unknown, lactulose-associated ischemic colitis is likely due to lactulose fermentation by gut bacteria leading to gaseous distention and subsequent increase in intraluminal pressure causing decreased intestinal blood flow and ischemia. Although this is a rare complication, patients undergoing lactulose therapy should be monitored closely, with signs of intestinal ischemia prompting further investigation as well as potentially holding lactulose to promote bowel rest.
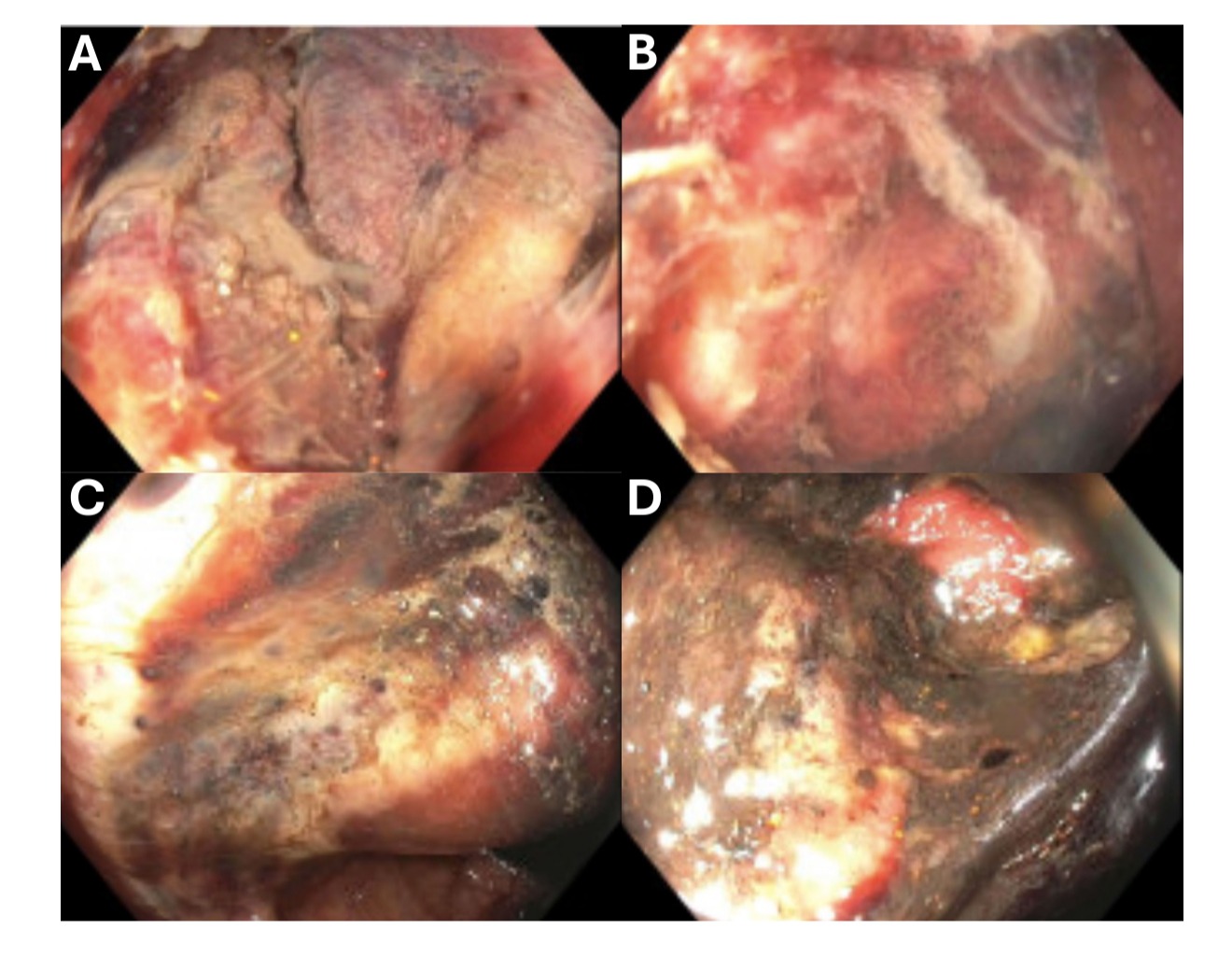
Figure: Extensive necrosis and erosion with mucosa ulceration in A) Sigmoid Colon, B) and C) Descending Colon, D) Transverse Colon.
Disclosures:
Sangkyu Noh indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
John Azizian indicated no relevant financial relationships.
Malini Chauhan indicated no relevant financial relationships.
Susana Escalante-Glorsky indicated no relevant financial relationships.
Sangkyu Noh, DO1, Samuel H. Cheong, DO1, Brandon Witten, MD2, Franklin Liu, MD1, John Azizian, MD1, Malini Chauhan, MD1, Susana Escalante-Glorsky, MD1. P2022 - Fermentation Fallout: A Case of Ischemic Colitis Triggered by Lactulose, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
