Monday Poster Session
Category: Colon
P2024 - A Rare Case of Melatonin Induced Microscopic Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JC
John Cooper, MD
University of Alabama at Birmingham Heersink School of Medicine
Birmingham, AL
Presenting Author(s)
John A. Cooper, MD1, Charles D. Evers, MD, MBA1, Osme Abdullah, MD1, Derek Estes, MD2
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
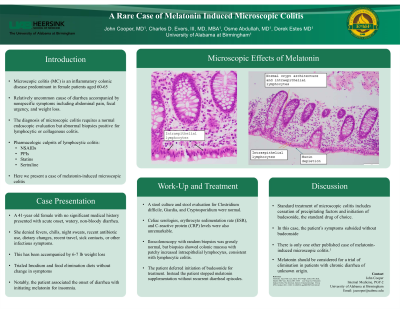
Introduction: Lymphocytic colitis, a variant of microscopic colitis, is a relatively uncommon cause of diarrhea. It can present insidiously or acutely with non-bloody, watery diarrhea accompanied by nonspecific symptoms including abdominal pain, fecal urgency, and weight loss. The endoscopic appearance of the colon is typically normal, but microscopic findings are characterized by ≥20 intraepithelial lymphocytes per 100 epithelial cells. Common pharmacologic culprits of lymphocytic colitis include non-steroidal anti-inflammatory drugs, proton-pump inhibitors, statins, and sertraline. Here, we present a case of lymphocytic colitis induced by melatonin.
Case Description/Methods: A 41-year old female with no significant medical history presented with acute onset, watery, non-bloody diarrhea. She denied fevers, chills, night sweats, weight loss, recent antibiotic use, dietary changes, recent travel, sick contacts, or other infectious symptoms. Notably, the patient associated the onset of diarrhea with initiating melatonin for insomnia. A stool culture and stool evaluation for Clostridium difficile, Giardia, and Cryptosporidium were normal. Celiac serologies, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were also unremarkable. Ileocolonoscopy with random biopsies was grossly normal, but biopsies showed colonic mucosa with patchy increased intraepithelial lymphocytes, consistent with lymphocytic colitis. Using shared-decision making, the patient and the healthcare team opted not to initiate budesonide for treatment. Instead, the patient ceased melatonin supplementation, leading to symptom resolution without recurrence of diarrheal episodes.
Discussion: Multiple etiologies of lymphocytic colitis exist including but not limited to environmental exposures, medications, and dietary changes. Multiple medications such as nonsteroidal anti-inflammatory drugs, proton-pump inhibitors, statins, selective serotonin reuptake inhibitors, and histamine H2-receptor blockers are known culprits of lymphocytic colitis. Through our literature review, this appears to be only the second documented case report of melatonin-induced lymphocytic colitis. Lymphocytic colitis differs from other causes of diarrhea in that it requires initiation of budesonide along with cessation of any precipitating medications, environmental factors, and dietary restrictions. In this case, symptoms resolved with just cessation of melatonin.
Disclosures:
John A. Cooper, MD1, Charles D. Evers, MD, MBA1, Osme Abdullah, MD1, Derek Estes, MD2. P2024 - A Rare Case of Melatonin Induced Microscopic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Lymphocytic colitis, a variant of microscopic colitis, is a relatively uncommon cause of diarrhea. It can present insidiously or acutely with non-bloody, watery diarrhea accompanied by nonspecific symptoms including abdominal pain, fecal urgency, and weight loss. The endoscopic appearance of the colon is typically normal, but microscopic findings are characterized by ≥20 intraepithelial lymphocytes per 100 epithelial cells. Common pharmacologic culprits of lymphocytic colitis include non-steroidal anti-inflammatory drugs, proton-pump inhibitors, statins, and sertraline. Here, we present a case of lymphocytic colitis induced by melatonin.
Case Description/Methods: A 41-year old female with no significant medical history presented with acute onset, watery, non-bloody diarrhea. She denied fevers, chills, night sweats, weight loss, recent antibiotic use, dietary changes, recent travel, sick contacts, or other infectious symptoms. Notably, the patient associated the onset of diarrhea with initiating melatonin for insomnia. A stool culture and stool evaluation for Clostridium difficile, Giardia, and Cryptosporidium were normal. Celiac serologies, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were also unremarkable. Ileocolonoscopy with random biopsies was grossly normal, but biopsies showed colonic mucosa with patchy increased intraepithelial lymphocytes, consistent with lymphocytic colitis. Using shared-decision making, the patient and the healthcare team opted not to initiate budesonide for treatment. Instead, the patient ceased melatonin supplementation, leading to symptom resolution without recurrence of diarrheal episodes.
Discussion: Multiple etiologies of lymphocytic colitis exist including but not limited to environmental exposures, medications, and dietary changes. Multiple medications such as nonsteroidal anti-inflammatory drugs, proton-pump inhibitors, statins, selective serotonin reuptake inhibitors, and histamine H2-receptor blockers are known culprits of lymphocytic colitis. Through our literature review, this appears to be only the second documented case report of melatonin-induced lymphocytic colitis. Lymphocytic colitis differs from other causes of diarrhea in that it requires initiation of budesonide along with cessation of any precipitating medications, environmental factors, and dietary restrictions. In this case, symptoms resolved with just cessation of melatonin.
Disclosures:
John Cooper indicated no relevant financial relationships.
Charles Evers indicated no relevant financial relationships.
Osme Abdullah indicated no relevant financial relationships.
Derek Estes indicated no relevant financial relationships.
John A. Cooper, MD1, Charles D. Evers, MD, MBA1, Osme Abdullah, MD1, Derek Estes, MD2. P2024 - A Rare Case of Melatonin Induced Microscopic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
