Monday Poster Session
Category: Colon
P1945 - Fecal Transplantation Improved Patients’ Reported Outcome After Immune Checkpoint Inhibitor Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YW
Yinghong Wang, MD, PhD
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Yinghong Wang, MD, PhD1, Malek Shatila, MD2, Krishnavathana Varatharajalu, MD2, Carolina Colli Cruz, MD3, Shu-En Shen, 2, Mary Herrera, 2, Xin Wang, PhD2, Anusha Thomas, MD2, Herbert DuPont, MD4
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4The University of Texas School of Public Health, Houston, TX
Introduction: Fecal microbiota transplantation (FMT) is effective for recurrent Clostridioides difficile infections (CDI). FMT has seen its application extended to other gastrointestinal disorders. Immune-mediated colitis (IMC) arises as a side effect of immune checkpoint inhibitor (ICI) therapy. Treatment of IMC is mostly limited to immunosuppressants, however refractory cases pose a significant challenge. FMT has been shown to be a successful treatment in refractory IMC in small case series, further large studies are needed to determine its efficacy.
Methods: We measured the efficacy of FMT for refractory IMC among 62 patients via chart review and clinical assessment and patients’ reported outcome (PRO) via established MD Anderson Symptom Inventory (MDASI). Among them, 9 patients had concurrent CDI as well at the time of diagnosis.
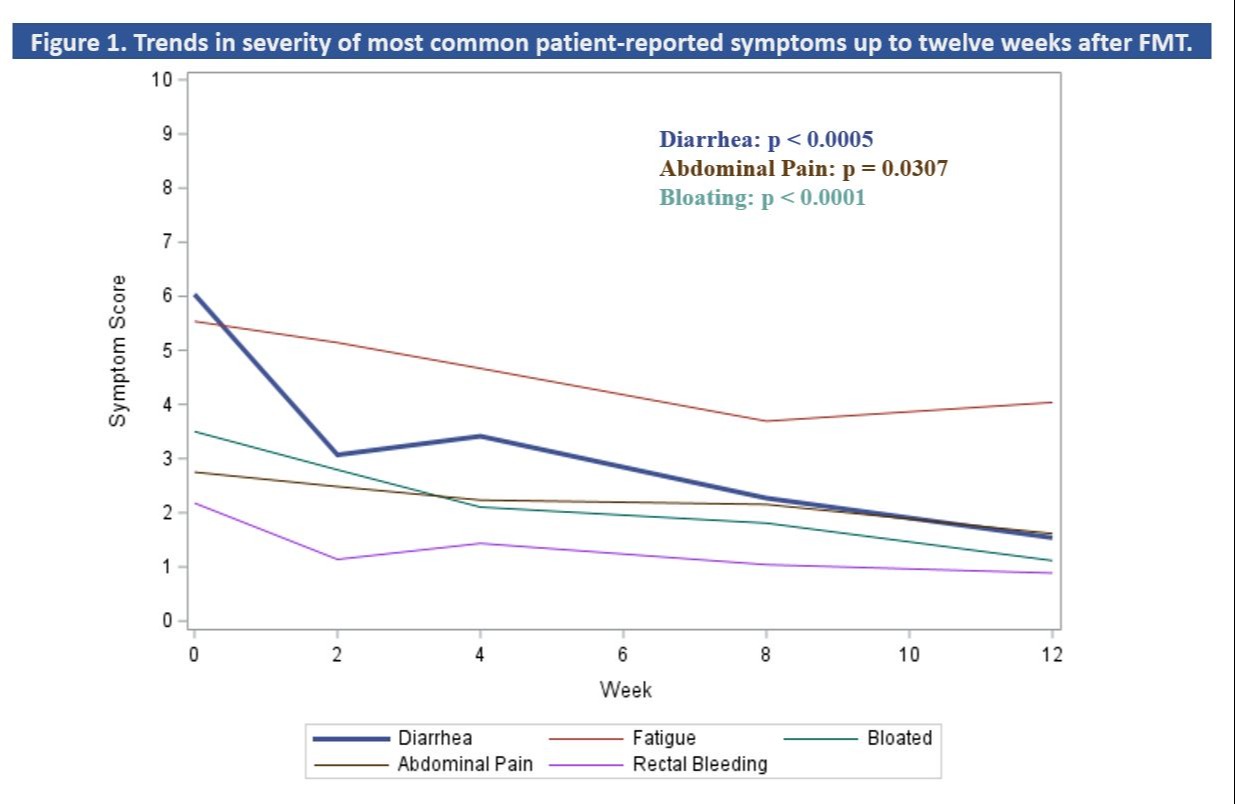
Results: Sixty-two patients were included in our study. Most patients had a peak diarrhea grade ≥ 3 (93.5%) and colitis grade ≥ 2 (87.1%). Ulcerous (29, 46.8%) and non-ulcerous (16, 25.8%) inflammation were the predominant endoscopic findings. Sixty (96.7%) patients received corticosteroids, and 58 patients (93.5%) received add-on infliximab or vedolizumab. IMC symptom response was 80.6% after FMT with median time to response of 5 days. The transient complication rate is 37% at 7 days and 27.4% at 30 days. Response rate among the 53 patients without concurrent CDI was 81.1%. Fifty (80.6%) patients demonstrated clinical remission by the end of the study period, and 12 (19.3%) were able to resume ICI treatment, and among them, 9 patients remained in remission. A total of 10 patients (16.1%) in our cohort developed recurrent colitis after FMT requiring immunosuppression; 3 of these recurrent cases were triggered by ICI resumption. On the PRO analysis, we observed a favorable trend of significant patient-reported symptom reduction on diarrhea (67.9% vs 11.5 %, p< 0.05) and abdominal bloating (32.1% vs 7.7%, p< 0.05) during 12 weeks after FMT. There was a 35.4 % reduction of moderate to severe symptoms with only 53.9% of patients reporting such symptoms after 12 weeks (down from 89.3%, p< 0.05) (Fig 1).
Discussion: FMT may serve as a potential treatment option in IMC refractory to standard treatment to avoid long-term steroid dependency and immunosuppression. It is effective to maintain IMC remission with a low complication rate. The role of the gut microbiome in cancer and the implications for FMT remain uncertain and need further elucidation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yinghong Wang, MD, PhD1, Malek Shatila, MD2, Krishnavathana Varatharajalu, MD2, Carolina Colli Cruz, MD3, Shu-En Shen, 2, Mary Herrera, 2, Xin Wang, PhD2, Anusha Thomas, MD2, Herbert DuPont, MD4. P1945 - Fecal Transplantation Improved Patients’ Reported Outcome After Immune Checkpoint Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4The University of Texas School of Public Health, Houston, TX
Introduction: Fecal microbiota transplantation (FMT) is effective for recurrent Clostridioides difficile infections (CDI). FMT has seen its application extended to other gastrointestinal disorders. Immune-mediated colitis (IMC) arises as a side effect of immune checkpoint inhibitor (ICI) therapy. Treatment of IMC is mostly limited to immunosuppressants, however refractory cases pose a significant challenge. FMT has been shown to be a successful treatment in refractory IMC in small case series, further large studies are needed to determine its efficacy.
Methods: We measured the efficacy of FMT for refractory IMC among 62 patients via chart review and clinical assessment and patients’ reported outcome (PRO) via established MD Anderson Symptom Inventory (MDASI). Among them, 9 patients had concurrent CDI as well at the time of diagnosis.
Results: Sixty-two patients were included in our study. Most patients had a peak diarrhea grade ≥ 3 (93.5%) and colitis grade ≥ 2 (87.1%). Ulcerous (29, 46.8%) and non-ulcerous (16, 25.8%) inflammation were the predominant endoscopic findings. Sixty (96.7%) patients received corticosteroids, and 58 patients (93.5%) received add-on infliximab or vedolizumab. IMC symptom response was 80.6% after FMT with median time to response of 5 days. The transient complication rate is 37% at 7 days and 27.4% at 30 days. Response rate among the 53 patients without concurrent CDI was 81.1%. Fifty (80.6%) patients demonstrated clinical remission by the end of the study period, and 12 (19.3%) were able to resume ICI treatment, and among them, 9 patients remained in remission. A total of 10 patients (16.1%) in our cohort developed recurrent colitis after FMT requiring immunosuppression; 3 of these recurrent cases were triggered by ICI resumption. On the PRO analysis, we observed a favorable trend of significant patient-reported symptom reduction on diarrhea (67.9% vs 11.5 %, p< 0.05) and abdominal bloating (32.1% vs 7.7%, p< 0.05) during 12 weeks after FMT. There was a 35.4 % reduction of moderate to severe symptoms with only 53.9% of patients reporting such symptoms after 12 weeks (down from 89.3%, p< 0.05) (Fig 1).
Discussion: FMT may serve as a potential treatment option in IMC refractory to standard treatment to avoid long-term steroid dependency and immunosuppression. It is effective to maintain IMC remission with a low complication rate. The role of the gut microbiome in cancer and the implications for FMT remain uncertain and need further elucidation.
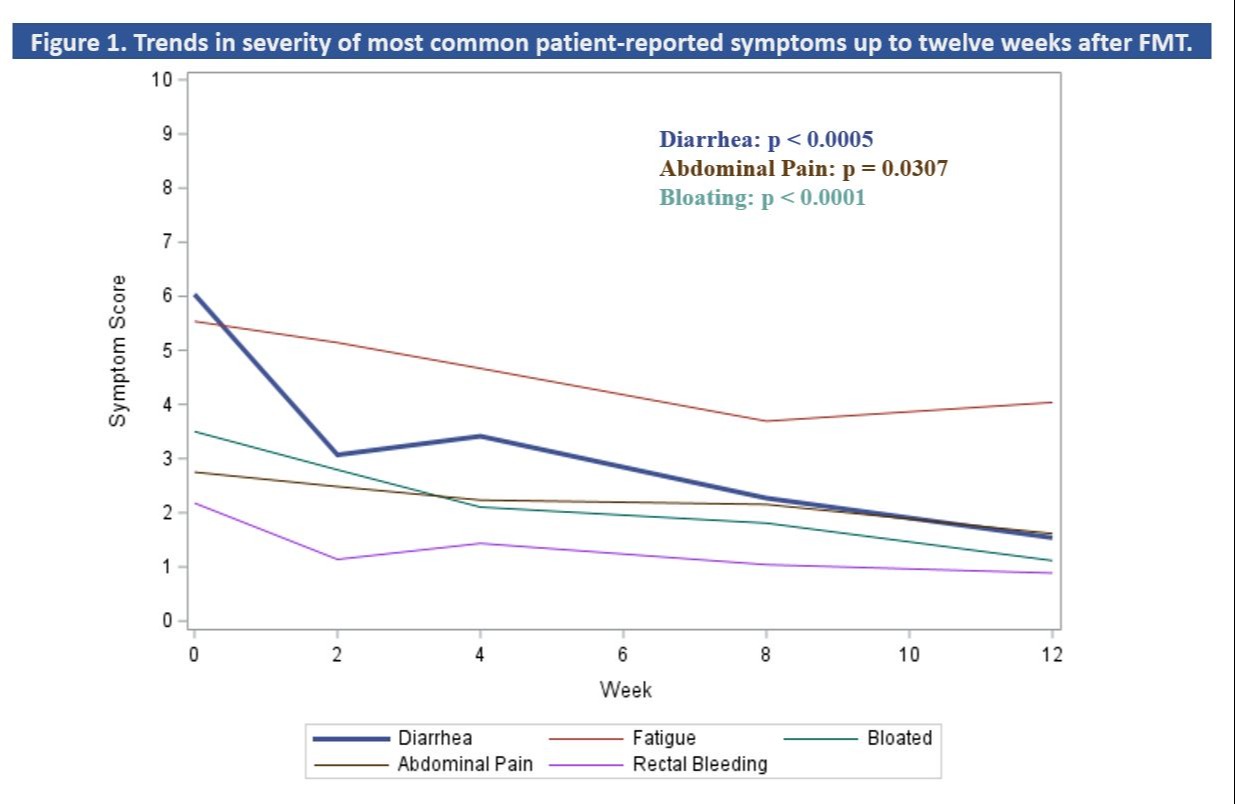
Figure: Figure 1
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Malek Shatila indicated no relevant financial relationships.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Shu-En Shen indicated no relevant financial relationships.
Mary Herrera indicated no relevant financial relationships.
Xin Wang indicated no relevant financial relationships.
Anusha Thomas indicated no relevant financial relationships.
Herbert DuPont indicated no relevant financial relationships.
Yinghong Wang, MD, PhD1, Malek Shatila, MD2, Krishnavathana Varatharajalu, MD2, Carolina Colli Cruz, MD3, Shu-En Shen, 2, Mary Herrera, 2, Xin Wang, PhD2, Anusha Thomas, MD2, Herbert DuPont, MD4. P1945 - Fecal Transplantation Improved Patients’ Reported Outcome After Immune Checkpoint Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
