Monday Poster Session
Category: Biliary/Pancreas
P1866 - Biliary Colonic Fistula in the Setting of Obstructive Cholelithiasis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Mushtaq, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Muhammad Mushtaq, DO, Ayesha Khan, DO, Minh Tran, MD, John Walker, MD, Sreeram Parupudi, MD
University of Texas Medical Branch, Galveston, TX
Introduction: Biliary enteric fistulas, a type of internal biliary fistula (IBF), are rare, with an incidence of 1% of patients with biliary disease1. Meanwhile, the incidence of cholecystocolic fistulas is approximately 0.06% to 0.14% in patients undergoing cholecystectomy. We present a case of cholecystocolic fistula developed in the context of obstructive cholelithiasis.
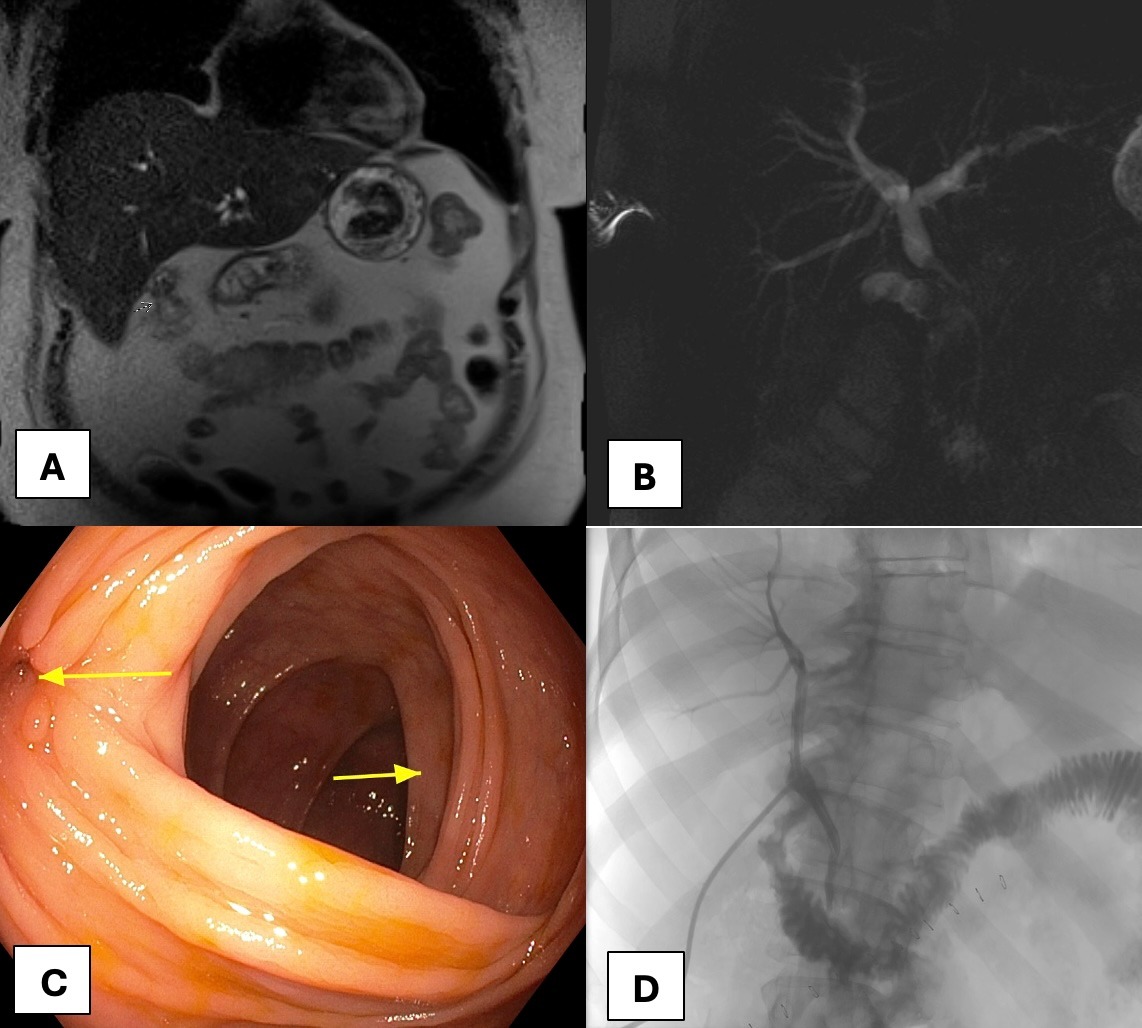
Case Description/Methods: A 60-year-old male with nausea, vomiting, and weight loss was admitted to an outside hospital for septic shock due to a suspected intra-abdominal infection and hyperbilirubinemia. Initial MRCP without contrast showed common bile duct (CBD) obstruction at the junction of the cystic duct with hepatic duct dilation. ERCP showed filling defects at the bifurcation of hepatic ducts. He was transferred to our facility to evaluate a possible mass. He denied a family history of malignancy. Lab work was remarkable for aspartate transaminase of 69 units/L, alanine transaminase of 77 units/L, alkaline phosphatase of 298 units/L, and total bilirubin of 1.3 mg/dL.
MRCP with contrast showed a mass effect on the common bile duct from the cystic duct due to multiple stones and possible fistulation between the gallbladder and the colon. The fistula site was endoscopically identified and marked. He had an open cholecystectomy and a resection of the colonic segment of the fistula with end-to-end anastomosis. The pathology report showed chronic cholecystitis and benign colonic tissue. Large stones impacted the gallbladder and compressed the CBD. After cholecystectomy, the biliary duct was repaired over a T-tube. Subsequent cholangiogram through the T-tube confirmed the patency of the biliary system with no biliary leak (Figure 1)
Discussion: The formation of internal biliary and cholecystocolic fistulas is thought to involve chronic gallbladder inflammation caused by gallstones and gradual erosion into the surrounding organs. Presentation varies from no or non-specific symptoms (abdominal pain, nausea, weight loss, or chronic diarrhea) to septic shock due to cholangitis. A high index of clinical suspicion is required to diagnose IBF. ERCP is the primary tool for diagnosis. Given the risk of imminent cholangitis and sepsis, prompt treatment is recommended. Cholecystectomy (open or laparoscopic) with the closure of the fistula (with or without segmental colonic resection) is considered the standard therapy for most patients.
Disclosures:
Muhammad Mushtaq, DO, Ayesha Khan, DO, Minh Tran, MD, John Walker, MD, Sreeram Parupudi, MD. P1866 - Biliary Colonic Fistula in the Setting of Obstructive Cholelithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Biliary enteric fistulas, a type of internal biliary fistula (IBF), are rare, with an incidence of 1% of patients with biliary disease1. Meanwhile, the incidence of cholecystocolic fistulas is approximately 0.06% to 0.14% in patients undergoing cholecystectomy. We present a case of cholecystocolic fistula developed in the context of obstructive cholelithiasis.
Case Description/Methods: A 60-year-old male with nausea, vomiting, and weight loss was admitted to an outside hospital for septic shock due to a suspected intra-abdominal infection and hyperbilirubinemia. Initial MRCP without contrast showed common bile duct (CBD) obstruction at the junction of the cystic duct with hepatic duct dilation. ERCP showed filling defects at the bifurcation of hepatic ducts. He was transferred to our facility to evaluate a possible mass. He denied a family history of malignancy. Lab work was remarkable for aspartate transaminase of 69 units/L, alanine transaminase of 77 units/L, alkaline phosphatase of 298 units/L, and total bilirubin of 1.3 mg/dL.
MRCP with contrast showed a mass effect on the common bile duct from the cystic duct due to multiple stones and possible fistulation between the gallbladder and the colon. The fistula site was endoscopically identified and marked. He had an open cholecystectomy and a resection of the colonic segment of the fistula with end-to-end anastomosis. The pathology report showed chronic cholecystitis and benign colonic tissue. Large stones impacted the gallbladder and compressed the CBD. After cholecystectomy, the biliary duct was repaired over a T-tube. Subsequent cholangiogram through the T-tube confirmed the patency of the biliary system with no biliary leak (Figure 1)
Discussion: The formation of internal biliary and cholecystocolic fistulas is thought to involve chronic gallbladder inflammation caused by gallstones and gradual erosion into the surrounding organs. Presentation varies from no or non-specific symptoms (abdominal pain, nausea, weight loss, or chronic diarrhea) to septic shock due to cholangitis. A high index of clinical suspicion is required to diagnose IBF. ERCP is the primary tool for diagnosis. Given the risk of imminent cholangitis and sepsis, prompt treatment is recommended. Cholecystectomy (open or laparoscopic) with the closure of the fistula (with or without segmental colonic resection) is considered the standard therapy for most patients.
Figure: A. Magnetic resonance cholangiopancreatography (MRCP ) shows a cholecystocolonic fistula between the gallbladder and the colonic hepatic flexure.
B. MRCP demonstrated intrahepatic and proximal extrahepatic biliary duct dilatation with abrupt cutoff due to an irregular filling defect of the proximal common bile duct.
C. Colonoscopy identified a fistula (left arrow) in the transverse colon at the hepatic flexure (right arrow).
D. Cholangiogram via the T-tube demonstrated a patent biliary system without evidence of biliary leakage, stricture, or enteric fistula.
B. MRCP demonstrated intrahepatic and proximal extrahepatic biliary duct dilatation with abrupt cutoff due to an irregular filling defect of the proximal common bile duct.
C. Colonoscopy identified a fistula (left arrow) in the transverse colon at the hepatic flexure (right arrow).
D. Cholangiogram via the T-tube demonstrated a patent biliary system without evidence of biliary leakage, stricture, or enteric fistula.
Disclosures:
Muhammad Mushtaq indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Minh Tran indicated no relevant financial relationships.
John Walker indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Muhammad Mushtaq, DO, Ayesha Khan, DO, Minh Tran, MD, John Walker, MD, Sreeram Parupudi, MD. P1866 - Biliary Colonic Fistula in the Setting of Obstructive Cholelithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
