Monday Poster Session
Category: Biliary/Pancreas
P1868 - Deciphering Deception: Pancreatic Mass Presenting as Post-Transplant Lymphoproliferative Disorder
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shivangini Duggal, MD
TTUHSC
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD2, Lakshmi Kattamur, MD2, Monica Botros, MD2, Raul Del Toro Mijares, MD2, Ricardo Badillo, MD1
1TTUHSC, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Post-Transplant Lymphoproliferative Disorder (PTLD) encompasses a range of diseases from benign lymphoid hyperplasia to aggressive lymphomas, primarily of B-cell origin and often associated with Epstein-Barr Virus (EBV). PTLD is a significant risk for solid organ transplant patients due to prolonged immunosuppression, typically occurring within the first year post-transplant or between 5-15 years later. Key risk factors include recipient EBV seronegativity, younger age, white ethnicity, closer HLA matching, and non-tacrolimus immunosuppressants.
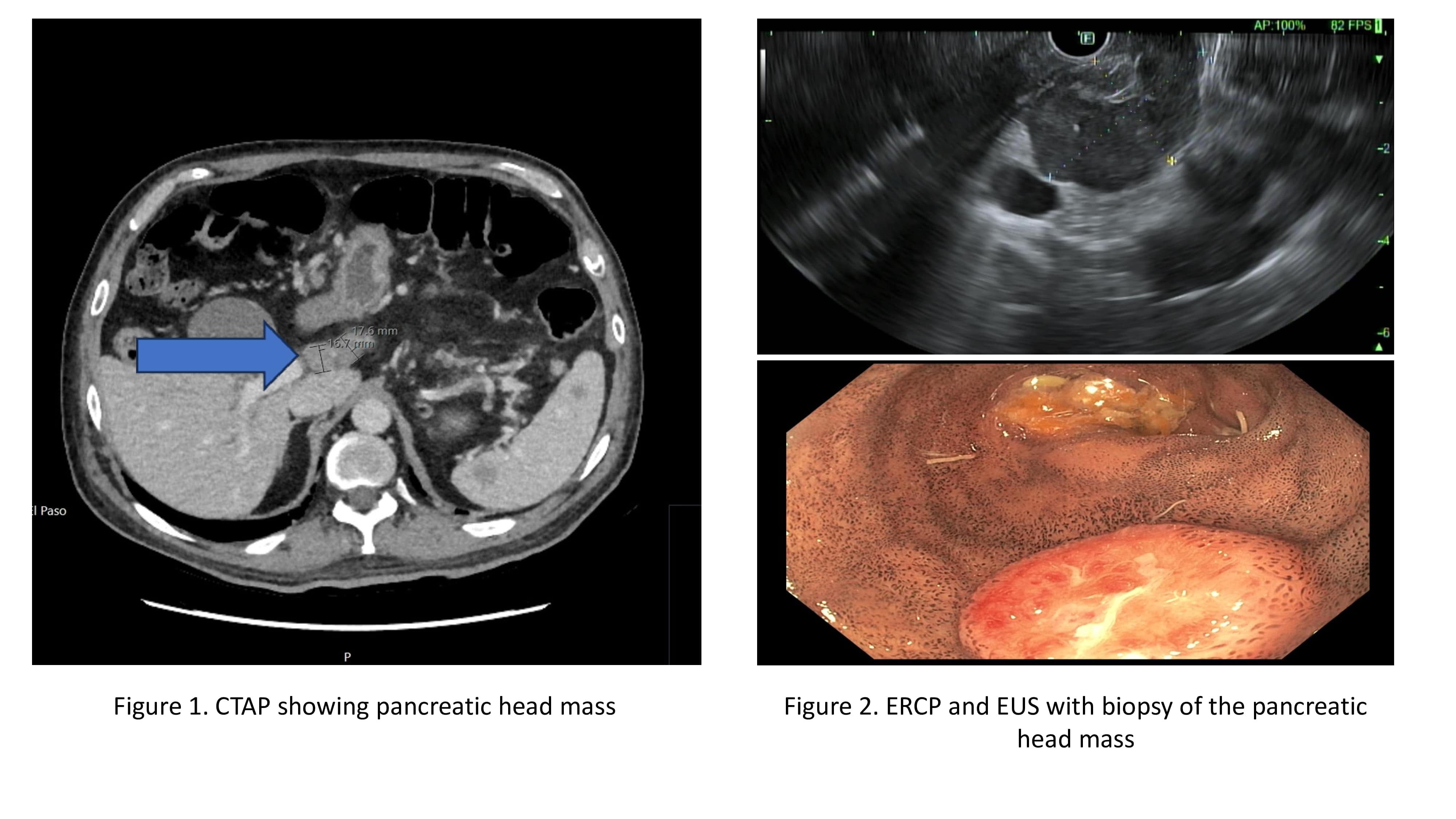
Case Description/Methods: A 68-year-old male with end-stage renal disease (ESRD) who had a renal transplant in 2013 presented with a 3-day history of nausea, vomiting, and poor oral intake. His medical history included type 2 diabetes (T2D) and hypertension (HTN). Examination revealed scleral icterus, supraclavicular lymphadenopathy, jaundice, and abdominal tenderness. Initial tests showed hyponatremia, elevated creatinine, direct hyperbilirubinemia, and elevated transaminases. A CT scan showed a mass in the head of the pancreas and a 7.6 cm mesenteric mass. A lymph node biopsy was negative for PTLD, but a pancreatic mass biopsy confirmed malignant diffuse large B-cell lymphoma (ABC type), indicating a rare PTLD presentation. Treatment included stopping mycophenolate and starting mini R-CHOP chemotherapy. Serology confirmed positive EBV IgG antibodies.
Discussion: The incidence of PTLD post-kidney transplant ranges from 0.8-2.5%, with 27% of cases involving the gastrointestinal tract. PTLD presentations vary widely, from asymptomatic to severe multiorgan failure. This case underscores the unusual presentation of PTLD as a pancreatic head mass with abdominal lymph node and mesenteric metastasis. Diagnosis involves PET/CT scans and targeted biopsies. Effective management requires a multidisciplinary approach, emphasizing early diagnosis and tailored treatment. Awareness of PTLD risk factors and maintaining clinical suspicion in transplant patients with atypical symptoms is crucial for timely intervention. This case highlights the importance of considering PTLD in differential diagnoses and the necessity of coordinated treatment strategies.
Disclosures:
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD2, Lakshmi Kattamur, MD2, Monica Botros, MD2, Raul Del Toro Mijares, MD2, Ricardo Badillo, MD1. P1868 - Deciphering Deception: Pancreatic Mass Presenting as Post-Transplant Lymphoproliferative Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TTUHSC, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Post-Transplant Lymphoproliferative Disorder (PTLD) encompasses a range of diseases from benign lymphoid hyperplasia to aggressive lymphomas, primarily of B-cell origin and often associated with Epstein-Barr Virus (EBV). PTLD is a significant risk for solid organ transplant patients due to prolonged immunosuppression, typically occurring within the first year post-transplant or between 5-15 years later. Key risk factors include recipient EBV seronegativity, younger age, white ethnicity, closer HLA matching, and non-tacrolimus immunosuppressants.
Case Description/Methods: A 68-year-old male with end-stage renal disease (ESRD) who had a renal transplant in 2013 presented with a 3-day history of nausea, vomiting, and poor oral intake. His medical history included type 2 diabetes (T2D) and hypertension (HTN). Examination revealed scleral icterus, supraclavicular lymphadenopathy, jaundice, and abdominal tenderness. Initial tests showed hyponatremia, elevated creatinine, direct hyperbilirubinemia, and elevated transaminases. A CT scan showed a mass in the head of the pancreas and a 7.6 cm mesenteric mass. A lymph node biopsy was negative for PTLD, but a pancreatic mass biopsy confirmed malignant diffuse large B-cell lymphoma (ABC type), indicating a rare PTLD presentation. Treatment included stopping mycophenolate and starting mini R-CHOP chemotherapy. Serology confirmed positive EBV IgG antibodies.
Discussion: The incidence of PTLD post-kidney transplant ranges from 0.8-2.5%, with 27% of cases involving the gastrointestinal tract. PTLD presentations vary widely, from asymptomatic to severe multiorgan failure. This case underscores the unusual presentation of PTLD as a pancreatic head mass with abdominal lymph node and mesenteric metastasis. Diagnosis involves PET/CT scans and targeted biopsies. Effective management requires a multidisciplinary approach, emphasizing early diagnosis and tailored treatment. Awareness of PTLD risk factors and maintaining clinical suspicion in transplant patients with atypical symptoms is crucial for timely intervention. This case highlights the importance of considering PTLD in differential diagnoses and the necessity of coordinated treatment strategies.
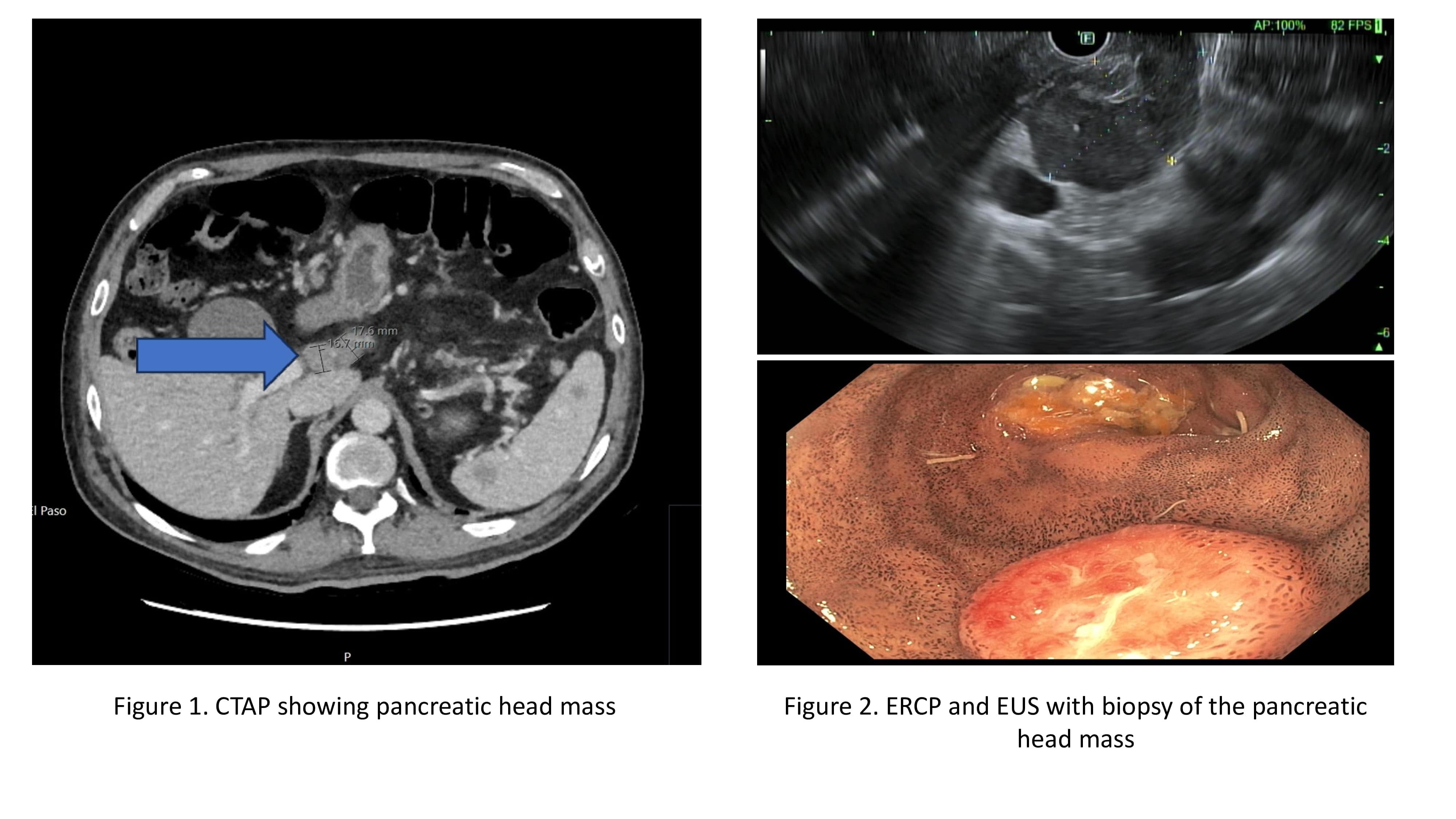
Figure: Figure 1. shows findings of the CT Abdomen and pelvis, highlighting pancreatic head mass
Figure 2. shows the EUS and ERCP findings, highlighting the pancreatic head mass, patient underwent pancreatic mass biopsy
Figure 2. shows the EUS and ERCP findings, highlighting the pancreatic head mass, patient underwent pancreatic mass biopsy
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Lakshmi Kattamur indicated no relevant financial relationships.
Monica Botros indicated no relevant financial relationships.
Raul Del Toro Mijares indicated no relevant financial relationships.
Ricardo Badillo indicated no relevant financial relationships.
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD2, Lakshmi Kattamur, MD2, Monica Botros, MD2, Raul Del Toro Mijares, MD2, Ricardo Badillo, MD1. P1868 - Deciphering Deception: Pancreatic Mass Presenting as Post-Transplant Lymphoproliferative Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
