Monday Poster Session
Category: Biliary/Pancreas
P1872 - Ketamine-Induced Cholangiopathy: A Rare Cause of Biliary Dilatation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shalva Eliava, MD
Englewood Hospital and Medical Center
Englewood, NJ
Presenting Author(s)
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Stephanie Rosales, MD1
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
Introduction: Ketamine is a synthetic compound that non-competitively inhibits NMDA receptors in the brain and is hepatically metabolized to its active form. It is commonly used for anesthesia, opioid-sparing analgesia, and resistant depression. We present a rare case of cholangiopathy associated with chronic use of ketamine at high doses.
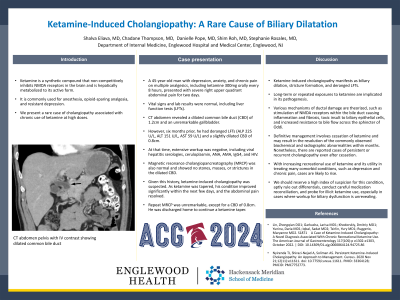
Case Description/Methods: A 45-year-old man with depression, anxiety, and chronic pain on multiple analgesics, including ketamine 300mg orally every 8 hours, presented with severe right upper quadrant abdominal pain for two days. Vital signs and lab results were normal, including liver function tests (LFTs). CT abdomen revealed a dilated common bile duct (CBD) of 1.2cm and an unremarkable gallbladder. However, six months prior, he had deranged LFTs (ALP 225 U/L, ALT 151 U/L, AST 59 U/L) and a slightly dilated CBD of 0.8cm. At that time, extensive workup was negative, including viral hepatitis serologies, ceruloplasmin, ANA, AMA, IgG4, and HIV. Magnetic resonance cholangiopancreatography (MRCP) was also normal and showed no stones, masses, or strictures in the dilated CBD. Given this history, ketamine-induced cholangiopathy was suspected. As ketamine was tapered, his condition improved significantly within the next few days, and the abdominal pain resolved. Repeat MRCP was unremarkable, except for a CBD of 0.8cm. He was discharged home to continue a ketamine taper.
Discussion: Ketamine-induced cholangiopathy manifests as biliary dilation, stricture formation, and deranged LFTs. Long-term or repeated exposures to ketamine are implicated in its pathogenesis. Various mechanisms of ductal damage are theorized, such as stimulation of NMDA receptors within the bile duct causing inflammation and fibrosis, toxic insult to biliary epithelial cells, and increased resistance to bile flow across the sphincter of Oddi. Definitive management involves cessation of ketamine and may result in the resolution of the commonly observed biochemical and radiographic abnormalities within months. Nonetheless, there are reported cases of persistent or recurrent cholangiopathy even after cessation. With increasing recreational use of ketamine and its utility in treating many comorbid conditions, such as depression and chronic pain, cases are likely to rise. We should reserve a high index of suspicion for this condition, aptly rule out differentials, conduct careful medication reconciliation, and probe for illicit ketamine use, especially in cases where workup for biliary dysfunction is unrevealing.
Disclosures:
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Stephanie Rosales, MD1. P1872 - Ketamine-Induced Cholangiopathy: A Rare Cause of Biliary Dilatation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
Introduction: Ketamine is a synthetic compound that non-competitively inhibits NMDA receptors in the brain and is hepatically metabolized to its active form. It is commonly used for anesthesia, opioid-sparing analgesia, and resistant depression. We present a rare case of cholangiopathy associated with chronic use of ketamine at high doses.
Case Description/Methods: A 45-year-old man with depression, anxiety, and chronic pain on multiple analgesics, including ketamine 300mg orally every 8 hours, presented with severe right upper quadrant abdominal pain for two days. Vital signs and lab results were normal, including liver function tests (LFTs). CT abdomen revealed a dilated common bile duct (CBD) of 1.2cm and an unremarkable gallbladder. However, six months prior, he had deranged LFTs (ALP 225 U/L, ALT 151 U/L, AST 59 U/L) and a slightly dilated CBD of 0.8cm. At that time, extensive workup was negative, including viral hepatitis serologies, ceruloplasmin, ANA, AMA, IgG4, and HIV. Magnetic resonance cholangiopancreatography (MRCP) was also normal and showed no stones, masses, or strictures in the dilated CBD. Given this history, ketamine-induced cholangiopathy was suspected. As ketamine was tapered, his condition improved significantly within the next few days, and the abdominal pain resolved. Repeat MRCP was unremarkable, except for a CBD of 0.8cm. He was discharged home to continue a ketamine taper.
Discussion: Ketamine-induced cholangiopathy manifests as biliary dilation, stricture formation, and deranged LFTs. Long-term or repeated exposures to ketamine are implicated in its pathogenesis. Various mechanisms of ductal damage are theorized, such as stimulation of NMDA receptors within the bile duct causing inflammation and fibrosis, toxic insult to biliary epithelial cells, and increased resistance to bile flow across the sphincter of Oddi. Definitive management involves cessation of ketamine and may result in the resolution of the commonly observed biochemical and radiographic abnormalities within months. Nonetheless, there are reported cases of persistent or recurrent cholangiopathy even after cessation. With increasing recreational use of ketamine and its utility in treating many comorbid conditions, such as depression and chronic pain, cases are likely to rise. We should reserve a high index of suspicion for this condition, aptly rule out differentials, conduct careful medication reconciliation, and probe for illicit ketamine use, especially in cases where workup for biliary dysfunction is unrevealing.
Disclosures:
Shalva Eliava indicated no relevant financial relationships.
Chadane Thompson indicated no relevant financial relationships.
Danielle Pope indicated no relevant financial relationships.
Shim Roh indicated no relevant financial relationships.
Stephanie Rosales indicated no relevant financial relationships.
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Stephanie Rosales, MD1. P1872 - Ketamine-Induced Cholangiopathy: A Rare Cause of Biliary Dilatation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
