Monday Poster Session
Category: Biliary/Pancreas
P1878 - Pancreatic Aftershock: Acute Pancreatitis With Recent Semaglutide Use
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rahul Borra, DO
HCA Healthcare
Presenting Author(s)
Rahul Borra, DO1, Thulfiqar Aljashamy, MD2, Jaafar Hamdan, MD2, Alisher Hamidullah, MD2
1HCA Healthcare, Lutz, FL; 2HCA Healthcare, Brooksville, FL
Introduction: The recent SUSTAIN-6 AND STEP 1 clinical trials have demonstrated GLP-1 agonists, including semaglutide, to be a breakthrough medication for the treatment of type 2 diabetes and weight loss. Here we present a case of acute pancreatitis in a patient with recent semaglutide use.
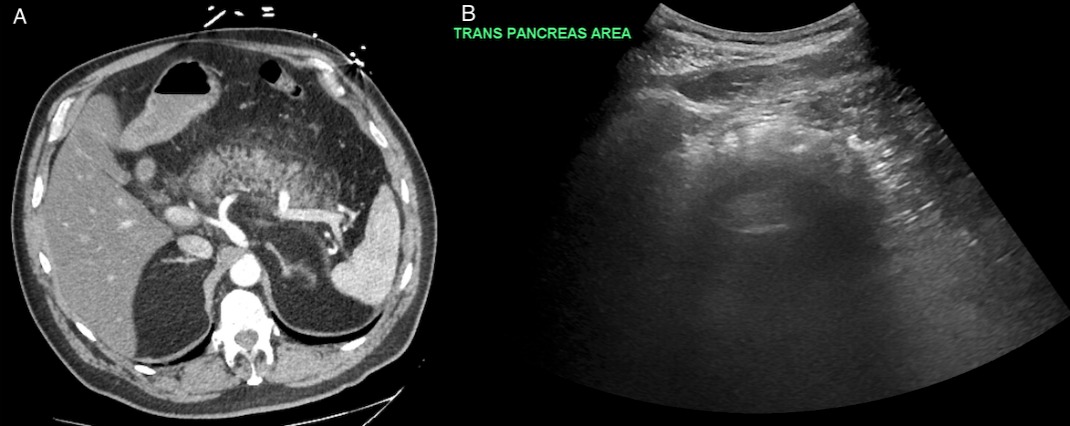
Case Description/Methods: The patient was a 67 year-old male with a past medical history of type 2 diabetes mellitus, hypertension and gastroesophageal reflux disease who presented with a chief complaint of sudden-onset abdominal pain with associated nausea. He stated that pain was localized to the upper abdomen, 10/10 in severity with radiation to the back and umbilicus. He also endorsed 4 episodes of non-bloody, non-bilious emesis. The patient was hypertensive at 182/88 on arrival. Lab work revealed a leukocytosis of 14.5. Liver functions were within normal limits, with AST 26 and ALT 48. Lipase was elevated at 1952. Calcium level was normal at 9.2. Lipid panel and autoimmune panel were unremarkable. CT abdomen/pelvis revealed peri-pancreatic fat stranding, consistent with pancreatitis. The patient was diagnosed with acute pancreatitis due to having 3/3 of the diagnostic criteria: characteristic abdominal pain, amylase and/or lipase greater than 3x upper limit of normal, and/or characteristic imaging findings. GI was consulted and subsequent MRCP did not reveal obstructing stones. Patient was continued on IV fluids and pain medication, with complete symptom resolution in two days. He was able to tolerate a regular diet. Patient was discharged with instruction to abstain from semaglutide and switch to another diabetic medication per PCP recommendation.
Discussion: GLP-1 agonists are becoming increasingly prescribed for type 2 diabetes mellitus due increased weight loss effects, decreased risk of hypoglycemia and ease of administration, leading to increased compliance. This class of medications mechanism of action of binding to GLP-1 receptors in the exocrine pancreas may directly lead to acute or chronic pancreatic inflammation. The SUSTAIN-6 trial demonstrated that there was no significant difference in the development of acute pancreatitis in patients on semaglutide vs placebo. However, potentially confounding this data is perhaps that patients with diabetes may present atypically, or that patients with diabetes may have other co-morbidities that increase the risk of developing acute pancreatitis. Nonetheless, the risk of developing pancreatitis with semaglutide use is a concern that practitioners should keep in mind.
Disclosures:
Rahul Borra, DO1, Thulfiqar Aljashamy, MD2, Jaafar Hamdan, MD2, Alisher Hamidullah, MD2. P1878 - Pancreatic Aftershock: Acute Pancreatitis With Recent Semaglutide Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Healthcare, Lutz, FL; 2HCA Healthcare, Brooksville, FL
Introduction: The recent SUSTAIN-6 AND STEP 1 clinical trials have demonstrated GLP-1 agonists, including semaglutide, to be a breakthrough medication for the treatment of type 2 diabetes and weight loss. Here we present a case of acute pancreatitis in a patient with recent semaglutide use.
Case Description/Methods: The patient was a 67 year-old male with a past medical history of type 2 diabetes mellitus, hypertension and gastroesophageal reflux disease who presented with a chief complaint of sudden-onset abdominal pain with associated nausea. He stated that pain was localized to the upper abdomen, 10/10 in severity with radiation to the back and umbilicus. He also endorsed 4 episodes of non-bloody, non-bilious emesis. The patient was hypertensive at 182/88 on arrival. Lab work revealed a leukocytosis of 14.5. Liver functions were within normal limits, with AST 26 and ALT 48. Lipase was elevated at 1952. Calcium level was normal at 9.2. Lipid panel and autoimmune panel were unremarkable. CT abdomen/pelvis revealed peri-pancreatic fat stranding, consistent with pancreatitis. The patient was diagnosed with acute pancreatitis due to having 3/3 of the diagnostic criteria: characteristic abdominal pain, amylase and/or lipase greater than 3x upper limit of normal, and/or characteristic imaging findings. GI was consulted and subsequent MRCP did not reveal obstructing stones. Patient was continued on IV fluids and pain medication, with complete symptom resolution in two days. He was able to tolerate a regular diet. Patient was discharged with instruction to abstain from semaglutide and switch to another diabetic medication per PCP recommendation.
Discussion: GLP-1 agonists are becoming increasingly prescribed for type 2 diabetes mellitus due increased weight loss effects, decreased risk of hypoglycemia and ease of administration, leading to increased compliance. This class of medications mechanism of action of binding to GLP-1 receptors in the exocrine pancreas may directly lead to acute or chronic pancreatic inflammation. The SUSTAIN-6 trial demonstrated that there was no significant difference in the development of acute pancreatitis in patients on semaglutide vs placebo. However, potentially confounding this data is perhaps that patients with diabetes may present atypically, or that patients with diabetes may have other co-morbidities that increase the risk of developing acute pancreatitis. Nonetheless, the risk of developing pancreatitis with semaglutide use is a concern that practitioners should keep in mind.
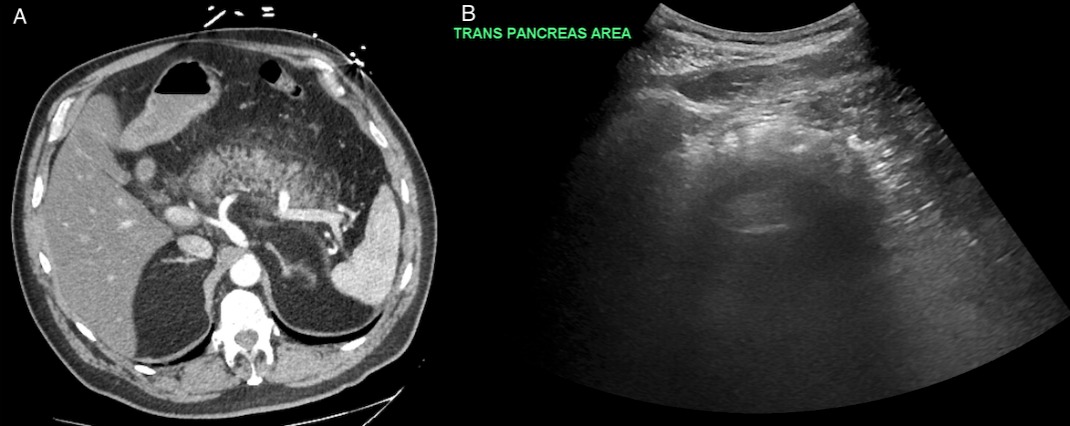
Figure: Figure A demonstrates CT Abdomen/Pelvis revealing edematous pancreas with abnormal fat stranding. Figure B shows right upper quadrant ultrasound revealing peri-pancreatic fluid.
Disclosures:
Rahul Borra indicated no relevant financial relationships.
Thulfiqar Aljashamy indicated no relevant financial relationships.
Jaafar Hamdan indicated no relevant financial relationships.
Alisher Hamidullah indicated no relevant financial relationships.
Rahul Borra, DO1, Thulfiqar Aljashamy, MD2, Jaafar Hamdan, MD2, Alisher Hamidullah, MD2. P1878 - Pancreatic Aftershock: Acute Pancreatitis With Recent Semaglutide Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
