Monday Poster Session
Category: Biliary/Pancreas
P1782 - Targeting Recurrences: Interventional Strategies to Curb Readmissions in Geriatric Biliary Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chun-Wei Pan, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Chun-Wei Pan, MD1, Daniel Guifarro, MD1, Bhanu SM. Pinnam, MD1, Yazan Abboud, MD2, Gautam Maddineni, MD3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Rutgers New Jersey Medical School, Newark, NJ; 3Florida State University, Cape Coral, FL
Introduction: Biliary pancreatitis is common in the elderly, and readmissions can be costly and detrimental. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic cholecystectomy are used to manage biliary pancreatitis, but their impact on readmission in the elderly is unclear. This study evaluates 30-day readmission rates in patients ≥65 years with biliary pancreatitis across different intervention strategies.
Methods: A retrospective analysis of the 2016-2019 Nationwide Readmission Database (NRD) was performed to identify patients aged 65 years and older with biliary pancreatitis. The primary aim was to determine the 30-day readmission rate among these patients and to compare readmission rates across different intervention groups during index admission: no intervention, ERCP only, laparoscopic cholecystectomy only, and both ERCP and laparoscopic cholecystectomy.
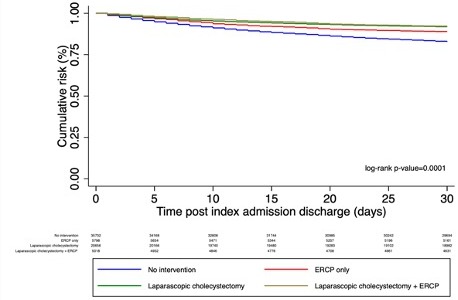
Results: Among 67,024 elderly patients with biliary pancreatitis, 53.17% received no intervention, 8.63% underwent ERCP only, 30.74% had laparoscopic cholecystectomy only, and 7.47% had both ERCP and laparoscopic cholecystectomy. The 30-day readmission rate was highest in the no-intervention group (17.19%) and lowest in the laparoscopic cholecystectomy+ERCP group (7.74%).
In unadjusted analyses, compared to no intervention, ERCP (Hazard Ratio (HR) 0.63, 95% Confidence interval (CI) 0.56-0.70), laparoscopic cholecystectomy (HR 0.46, 95% CI 0.43-0.49), and ERCP plus laparoscopic cholecystectomy (HR 0.43, 95% CI 0.37-0.50) were associated with significantly lower hazards of readmission. After adjustment for patient factors, these associations remained significant, with adjusted hazard ratios of 0.65 (95% CI 0.58-0.73), 0.52 (95% CI 0.48-0.56), and 0.47 (95% CI 0.40-0.54), respectively.
Charlson Comorbidity Index was a strong predictor of readmission, with adjusted hazard ratios of 1.24 (95% CI 1.11-1.37), 1.44 (95% CI 1.29-1.60), and 2.02 (95% CI 1.84-2.23) for scores of 1, 2, and >3, respectively, compared to a score of 0. Readmissions occurred an average of 9-12 days post-discharge across intervention groups.
Discussion: In elderly patients with biliary pancreatitis, 30-day readmission varied significantly across intervention groups. Even in this population with higher comorbidity burden, ERCP and laparoscopic cholecystectomy, alone or combined, were associated with lower readmission compared to no intervention during the index admission. Timely intervention may reduce readmissions in this vulnerable population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chun-Wei Pan, MD1, Daniel Guifarro, MD1, Bhanu SM. Pinnam, MD1, Yazan Abboud, MD2, Gautam Maddineni, MD3. P1782 - Targeting Recurrences: Interventional Strategies to Curb Readmissions in Geriatric Biliary Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Rutgers New Jersey Medical School, Newark, NJ; 3Florida State University, Cape Coral, FL
Introduction: Biliary pancreatitis is common in the elderly, and readmissions can be costly and detrimental. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic cholecystectomy are used to manage biliary pancreatitis, but their impact on readmission in the elderly is unclear. This study evaluates 30-day readmission rates in patients ≥65 years with biliary pancreatitis across different intervention strategies.
Methods: A retrospective analysis of the 2016-2019 Nationwide Readmission Database (NRD) was performed to identify patients aged 65 years and older with biliary pancreatitis. The primary aim was to determine the 30-day readmission rate among these patients and to compare readmission rates across different intervention groups during index admission: no intervention, ERCP only, laparoscopic cholecystectomy only, and both ERCP and laparoscopic cholecystectomy.
Results: Among 67,024 elderly patients with biliary pancreatitis, 53.17% received no intervention, 8.63% underwent ERCP only, 30.74% had laparoscopic cholecystectomy only, and 7.47% had both ERCP and laparoscopic cholecystectomy. The 30-day readmission rate was highest in the no-intervention group (17.19%) and lowest in the laparoscopic cholecystectomy+ERCP group (7.74%).
In unadjusted analyses, compared to no intervention, ERCP (Hazard Ratio (HR) 0.63, 95% Confidence interval (CI) 0.56-0.70), laparoscopic cholecystectomy (HR 0.46, 95% CI 0.43-0.49), and ERCP plus laparoscopic cholecystectomy (HR 0.43, 95% CI 0.37-0.50) were associated with significantly lower hazards of readmission. After adjustment for patient factors, these associations remained significant, with adjusted hazard ratios of 0.65 (95% CI 0.58-0.73), 0.52 (95% CI 0.48-0.56), and 0.47 (95% CI 0.40-0.54), respectively.
Charlson Comorbidity Index was a strong predictor of readmission, with adjusted hazard ratios of 1.24 (95% CI 1.11-1.37), 1.44 (95% CI 1.29-1.60), and 2.02 (95% CI 1.84-2.23) for scores of 1, 2, and >3, respectively, compared to a score of 0. Readmissions occurred an average of 9-12 days post-discharge across intervention groups.
Discussion: In elderly patients with biliary pancreatitis, 30-day readmission varied significantly across intervention groups. Even in this population with higher comorbidity burden, ERCP and laparoscopic cholecystectomy, alone or combined, were associated with lower readmission compared to no intervention during the index admission. Timely intervention may reduce readmissions in this vulnerable population.
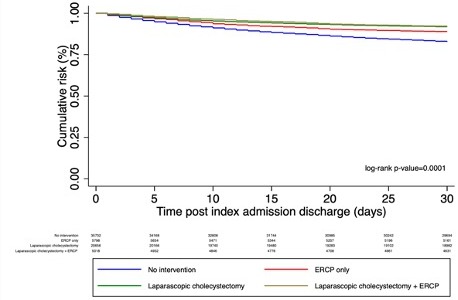
Figure: Kaplan-Meier curve of 30-day all-cause readmission risk, stratify by interventional groups in elderly patient admitted for Biliary pancreatitis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chun-Wei Pan indicated no relevant financial relationships.
Daniel Guifarro indicated no relevant financial relationships.
Bhanu Pinnam indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Chun-Wei Pan, MD1, Daniel Guifarro, MD1, Bhanu SM. Pinnam, MD1, Yazan Abboud, MD2, Gautam Maddineni, MD3. P1782 - Targeting Recurrences: Interventional Strategies to Curb Readmissions in Geriatric Biliary Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
