Monday Poster Session
Category: Biliary/Pancreas
P1785 - Intraductal Papillary Neoplasm of the Bile Duct: A Rare Precursor of Invasive Cholangiocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jiteshwar S. Pannu, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Jiteshwar S. Pannu, MD1, Andrea Fernandez, MD1, Elizabeth Manion, MD2, Shruti Mony, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2MAWD Pathology Group, Lenexa, KS
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are rare neoplasms of the biliary tree, characterized by intraluminal papillary growth and are often described as the biliary counterparts of intraductal papillary mucinous neoplasms (IPMNs) of the pancreas. Herein, we present a rare case of an elderly male with obstructive jaundice, who was found to have a left hepatic IPNB.
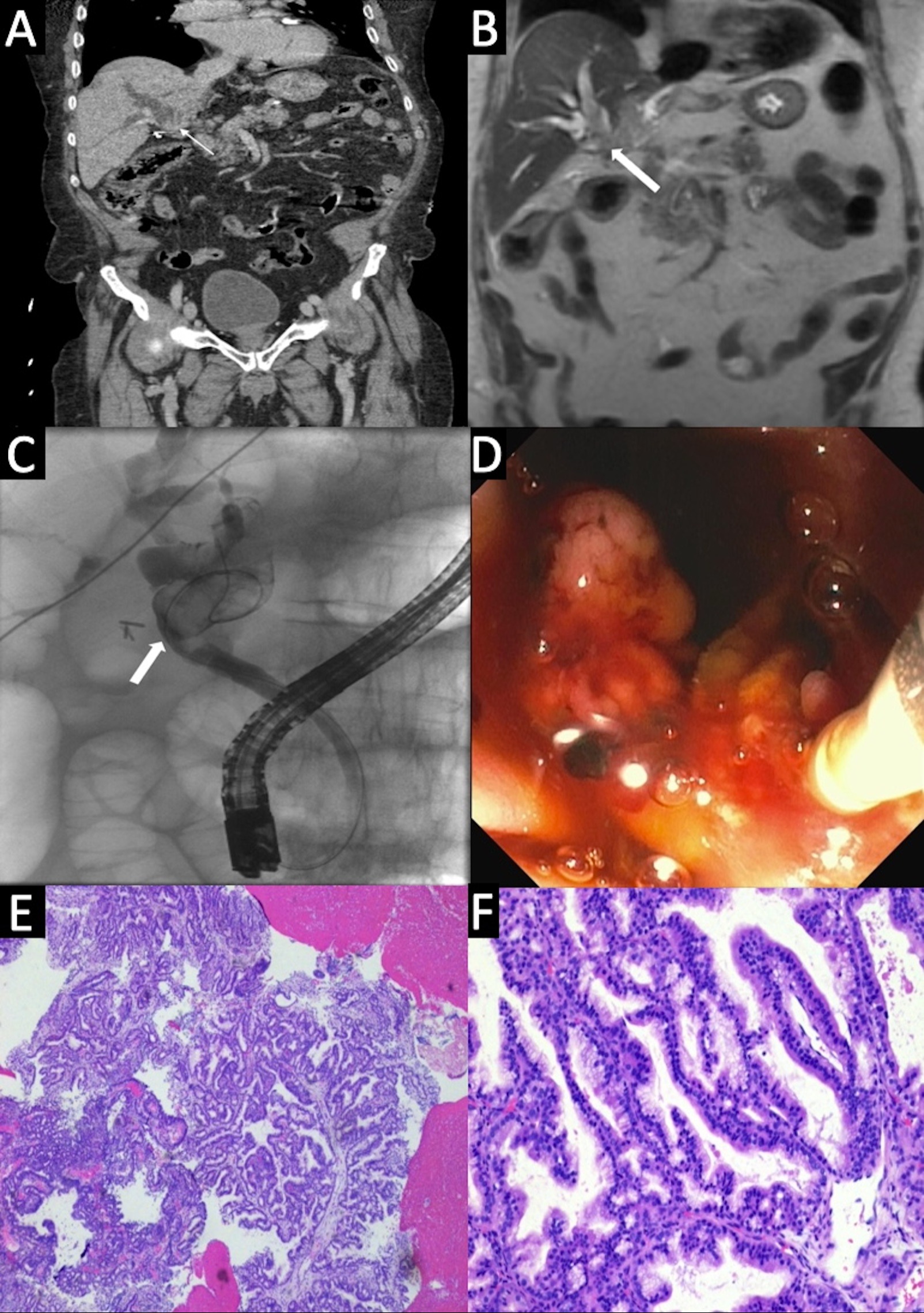
Case Description/Methods: An 81-year-old male with a history of neurofibromatosis 1 (NF1) presented with itching, jaundice and fatigue for 1 week. Physical exam revealed scleral icterus and skin excoriations. Labs demonstrated cholestasis with T. bilirubin 12, AST 195, ALT 197, ALP 400. CT Abdomen with contrast showed moderate intrahepatic biliary (IHB) dilation due to a left hepatic lobe mass. This was further characterized on MRCP as an ill-defined, intra-luminal biliary mass, encroaching upon the IHB ductal confluence with upstream dilation. A subsequent ERCP confirmed multiple intraductal biliary polypoid lesions resulting in upstream obstruction. On balloon sweeps, chunks of polypoid tissue, presumably tumor fragments were swept from the biliary tree. A plastic stent was deployed. Histopathological analysis revealed tubulo-papillary epithelial proliferation consistent with IPNB (biliary type) without dysplasia/malignancy. A multi-disciplinary discussion concluded the patient to be high risk for surgical interventions and a consensus was made to continue symptomatic management of biliary obstruction with endoscopic/percutaneous drainage.
Discussion: Due to their low prevalence (5-15% amongst biliary tumors), accurate preoperative diagnosis of IPNBs is challenging. Known risk factors include hepatolithiasis, clonorchiasis, PSC, biliary malformations, FAP and Gardner Syndrome. Our case is unique as there is no known association of IPNBs and NF1. IPNBs can result in biliary obstruction due to mucin hypersecretion, bleeding, cholangitis, and malignant transformation. Diagnosis typically relies on imaging such as CT, MRI and ERCP with cholangioscopy, coupled with histopathological confirmation. Based on the degree of dysplasia, IPNBs can be classified as low-to-intermediate and high grade. Treatment strategies vary from surveillance for low-grade lesions to surgical resection for select patients with high grade dysplasia and carcinoma. The role of endoscopic interventions includes biliary stenting and drainage, trans-papillary intraluminal radiotherapy and radio-frequency ablation as alternative palliative modalities.
Disclosures:
Jiteshwar S. Pannu, MD1, Andrea Fernandez, MD1, Elizabeth Manion, MD2, Shruti Mony, MD1. P1785 - Intraductal Papillary Neoplasm of the Bile Duct: A Rare Precursor of Invasive Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2MAWD Pathology Group, Lenexa, KS
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are rare neoplasms of the biliary tree, characterized by intraluminal papillary growth and are often described as the biliary counterparts of intraductal papillary mucinous neoplasms (IPMNs) of the pancreas. Herein, we present a rare case of an elderly male with obstructive jaundice, who was found to have a left hepatic IPNB.
Case Description/Methods: An 81-year-old male with a history of neurofibromatosis 1 (NF1) presented with itching, jaundice and fatigue for 1 week. Physical exam revealed scleral icterus and skin excoriations. Labs demonstrated cholestasis with T. bilirubin 12, AST 195, ALT 197, ALP 400. CT Abdomen with contrast showed moderate intrahepatic biliary (IHB) dilation due to a left hepatic lobe mass. This was further characterized on MRCP as an ill-defined, intra-luminal biliary mass, encroaching upon the IHB ductal confluence with upstream dilation. A subsequent ERCP confirmed multiple intraductal biliary polypoid lesions resulting in upstream obstruction. On balloon sweeps, chunks of polypoid tissue, presumably tumor fragments were swept from the biliary tree. A plastic stent was deployed. Histopathological analysis revealed tubulo-papillary epithelial proliferation consistent with IPNB (biliary type) without dysplasia/malignancy. A multi-disciplinary discussion concluded the patient to be high risk for surgical interventions and a consensus was made to continue symptomatic management of biliary obstruction with endoscopic/percutaneous drainage.
Discussion: Due to their low prevalence (5-15% amongst biliary tumors), accurate preoperative diagnosis of IPNBs is challenging. Known risk factors include hepatolithiasis, clonorchiasis, PSC, biliary malformations, FAP and Gardner Syndrome. Our case is unique as there is no known association of IPNBs and NF1. IPNBs can result in biliary obstruction due to mucin hypersecretion, bleeding, cholangitis, and malignant transformation. Diagnosis typically relies on imaging such as CT, MRI and ERCP with cholangioscopy, coupled with histopathological confirmation. Based on the degree of dysplasia, IPNBs can be classified as low-to-intermediate and high grade. Treatment strategies vary from surveillance for low-grade lesions to surgical resection for select patients with high grade dysplasia and carcinoma. The role of endoscopic interventions includes biliary stenting and drainage, trans-papillary intraluminal radiotherapy and radio-frequency ablation as alternative palliative modalities.
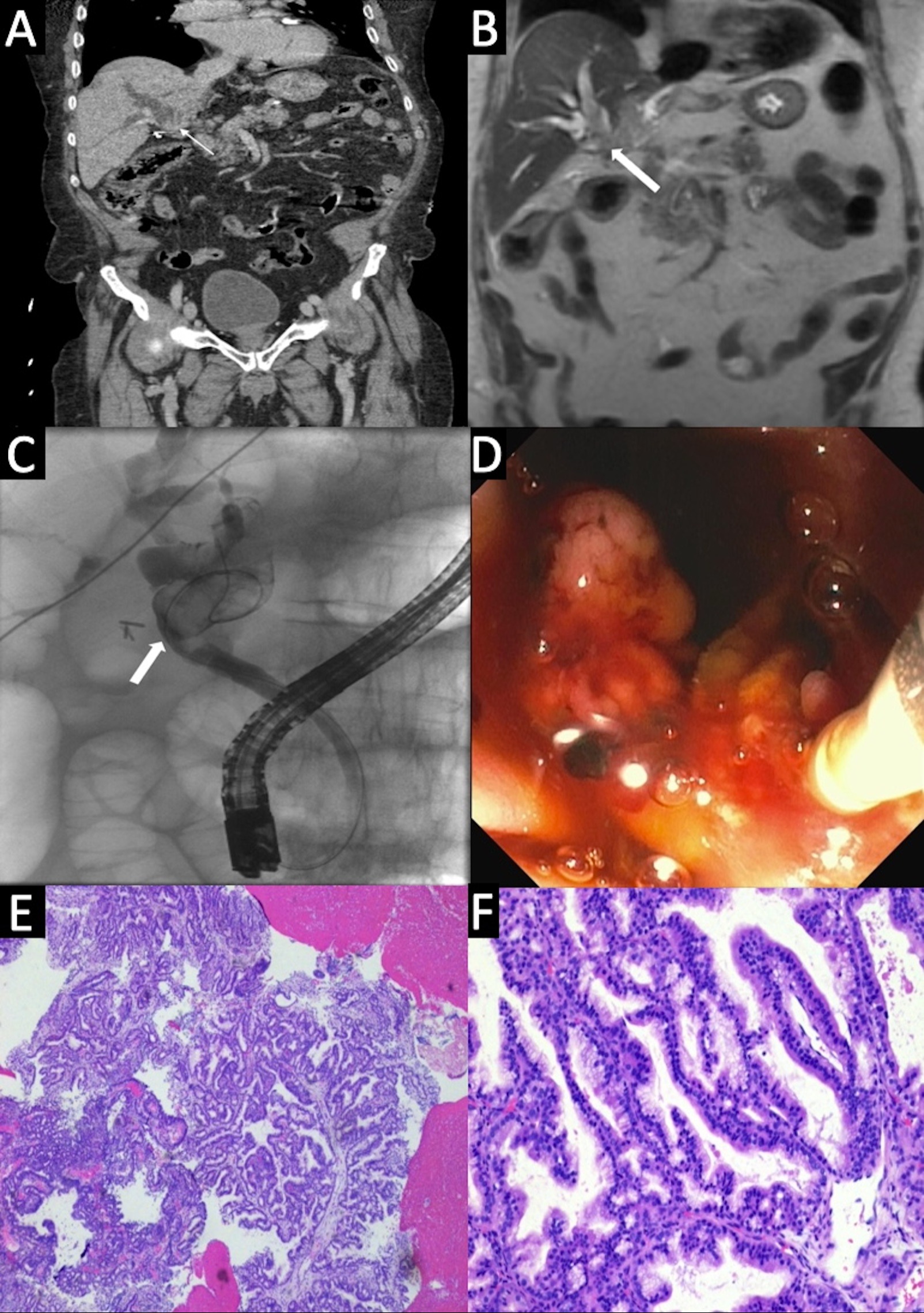
Figure: Figure A: CT Abdomen with contrast showing moderate intra-hepatic biliary (IHB) dilation with concern for a mass in the left hepatic lobe;
Figure B: MRCP showing ill-defined, intra-luminal biliary mass, encroaching upon the IHB ductal confluence with upstream dilation;
Figure C: ERCP with multiple intra-ductal biliary polypoid lesions resulting in upstream obstruction;
Figure D: Multiple chunks of polypoid tissue (presumably tumor fragments) swept from the biliary tree with surrounding bleeding;
Figure E/F: Histopathological analysis showing tubulo-papillary epithelial proliferation consistent with IPNB (biliary type) without dysplasia or malignancy
Figure B: MRCP showing ill-defined, intra-luminal biliary mass, encroaching upon the IHB ductal confluence with upstream dilation;
Figure C: ERCP with multiple intra-ductal biliary polypoid lesions resulting in upstream obstruction;
Figure D: Multiple chunks of polypoid tissue (presumably tumor fragments) swept from the biliary tree with surrounding bleeding;
Figure E/F: Histopathological analysis showing tubulo-papillary epithelial proliferation consistent with IPNB (biliary type) without dysplasia or malignancy
Disclosures:
Jiteshwar Pannu indicated no relevant financial relationships.
Andrea Fernandez indicated no relevant financial relationships.
Elizabeth Manion indicated no relevant financial relationships.
Shruti Mony indicated no relevant financial relationships.
Jiteshwar S. Pannu, MD1, Andrea Fernandez, MD1, Elizabeth Manion, MD2, Shruti Mony, MD1. P1785 - Intraductal Papillary Neoplasm of the Bile Duct: A Rare Precursor of Invasive Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
