Monday Poster Session
Category: Biliary/Pancreas
P1796 - Untangled Mystery: Peutz-Jeghers Syndrome Unmasked by Pancreatic Intussusception
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MD
Manuel Del Rio-Montesinos, MD
VA Caribbean Healthcare System
San Juan, Puerto Rico
Presenting Author(s)
Award: Presidential Poster Award
Manuel Del Rio-Montesinos, MD1, Viviana Blanco, MD2, Pablo Costas, MD3, Joan Neptune-Rosa, BS4
1VA Caribbean Healthcare System, San Juan, Puerto Rico; 2University of Puerto Rico Medical Sciences Campus, Coto Laurel, Puerto Rico; 3University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 4Universidad Central del Caribe School of Medicine, San Juan, Puerto Rico
Introduction: Peutz-Jeghers Syndrome(PJS) is a hereditary condition that increases susceptibility to various cancers. It involves germline STK11 mutations and often an acquired defect in the second STK11 allele in somatic cells. The STK11/LKB1 gene acts as a tumor suppressor, crucial for cell cycle regulation. Its incidence ranges from 1 in 25,000 to 300,000, affecting both sexes equally. This syndrome raises the risk of ovarian, uterine, cervical, breast, testicular, pancreatic, stomach, and colorectal cancers. Over 95% of patients have mucocutaneous dark blue macules, mainly on the lips. The typical presentation is bowel obstruction from hamartomatous polyps. We report an atypical late-onset case, where a duodenal polyp led to pancreatic intussusception.
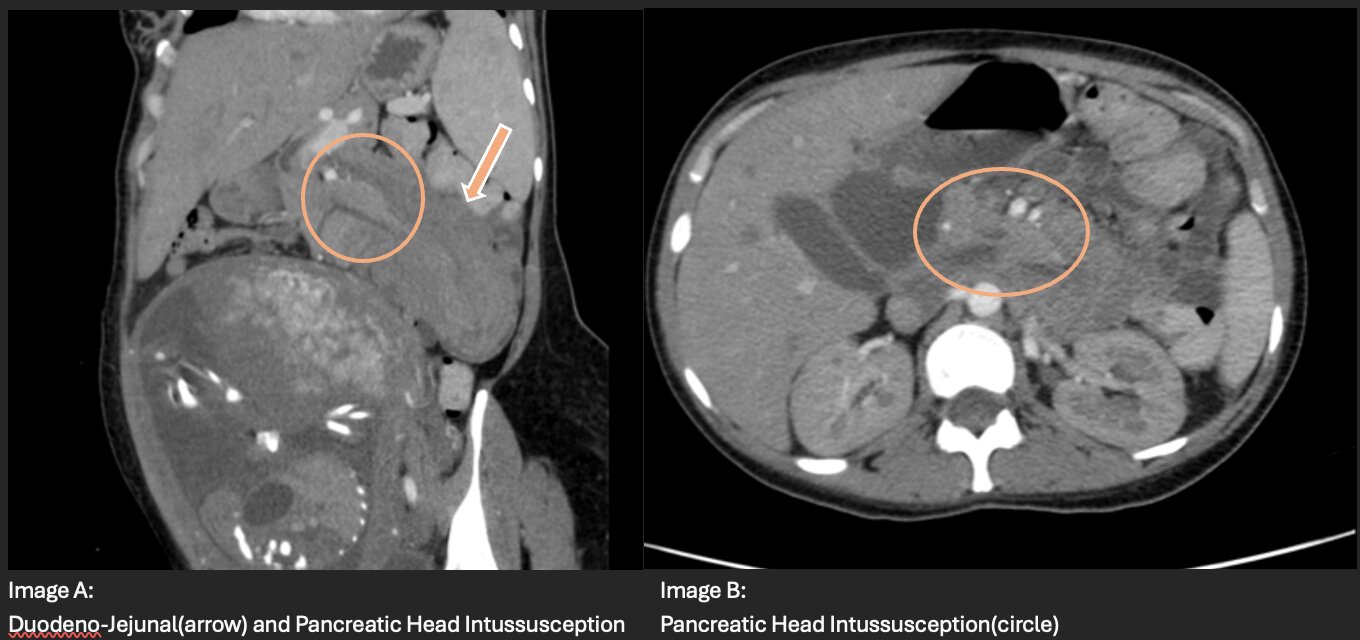
Case Description/Methods: A 32-year-old pregnant woman presents with nausea, vomiting, elevated liver and pancreatic enzymes. She also has abdominal distension and inability to pass flatus. Her paternal grandmother had breast and colon cancer. She reports similar episodes managed as acute pancreatitis. Physical examination reveals a distended, non-tender abdomen. Laboratory shows elevated amylase (1222 U/L), lipase (632 U/L), and total bilirubin (2.24 mg/dL). Abdominal sonogram shows a dilated common bile duct and dilated pancreatic duct. A subsequent abdominopelvic CT scan reveals a large duodenojejunal intussusception, with intussusception of the pancreatic head and uncinate process. Upper endoscopy identified a 5 cm villous mass from the second portion of the duodenum, attached by a pseudo-stalk, causing transient pancreatic outflow obstruction. Advancement of endoscope led to transient resolve of intussusception.
Discussion: PJS is associated with colonic polyps' development in the second decade of life. Common presentations include microcytic anemia and intestinal intussusception, leading to obstruction. Bowel obstruction requires surgical intervention preferably in the second trimester for pregnant patients. This case is distinctive due to concomitant pancreatic intussusception, an unusual finding in a patient without pancreatic malformation. Isolated elevation in amylase and lipase should prompt clinicians to suspect pancreatic outflow tract obstruction. Patients with PJS have an increased risk of various cancers, notably colorectal cancer. Surveillance colonoscopy should begin at age 8, with polypectomy or surgical referral if polyps are numerous. Female patients require annual screenings for breast, uterine, ovarian, and cervical cancer.
Disclosures:
Manuel Del Rio-Montesinos, MD1, Viviana Blanco, MD2, Pablo Costas, MD3, Joan Neptune-Rosa, BS4. P1796 - Untangled Mystery: Peutz-Jeghers Syndrome Unmasked by Pancreatic Intussusception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Manuel Del Rio-Montesinos, MD1, Viviana Blanco, MD2, Pablo Costas, MD3, Joan Neptune-Rosa, BS4
1VA Caribbean Healthcare System, San Juan, Puerto Rico; 2University of Puerto Rico Medical Sciences Campus, Coto Laurel, Puerto Rico; 3University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 4Universidad Central del Caribe School of Medicine, San Juan, Puerto Rico
Introduction: Peutz-Jeghers Syndrome(PJS) is a hereditary condition that increases susceptibility to various cancers. It involves germline STK11 mutations and often an acquired defect in the second STK11 allele in somatic cells. The STK11/LKB1 gene acts as a tumor suppressor, crucial for cell cycle regulation. Its incidence ranges from 1 in 25,000 to 300,000, affecting both sexes equally. This syndrome raises the risk of ovarian, uterine, cervical, breast, testicular, pancreatic, stomach, and colorectal cancers. Over 95% of patients have mucocutaneous dark blue macules, mainly on the lips. The typical presentation is bowel obstruction from hamartomatous polyps. We report an atypical late-onset case, where a duodenal polyp led to pancreatic intussusception.
Case Description/Methods: A 32-year-old pregnant woman presents with nausea, vomiting, elevated liver and pancreatic enzymes. She also has abdominal distension and inability to pass flatus. Her paternal grandmother had breast and colon cancer. She reports similar episodes managed as acute pancreatitis. Physical examination reveals a distended, non-tender abdomen. Laboratory shows elevated amylase (1222 U/L), lipase (632 U/L), and total bilirubin (2.24 mg/dL). Abdominal sonogram shows a dilated common bile duct and dilated pancreatic duct. A subsequent abdominopelvic CT scan reveals a large duodenojejunal intussusception, with intussusception of the pancreatic head and uncinate process. Upper endoscopy identified a 5 cm villous mass from the second portion of the duodenum, attached by a pseudo-stalk, causing transient pancreatic outflow obstruction. Advancement of endoscope led to transient resolve of intussusception.
Discussion: PJS is associated with colonic polyps' development in the second decade of life. Common presentations include microcytic anemia and intestinal intussusception, leading to obstruction. Bowel obstruction requires surgical intervention preferably in the second trimester for pregnant patients. This case is distinctive due to concomitant pancreatic intussusception, an unusual finding in a patient without pancreatic malformation. Isolated elevation in amylase and lipase should prompt clinicians to suspect pancreatic outflow tract obstruction. Patients with PJS have an increased risk of various cancers, notably colorectal cancer. Surveillance colonoscopy should begin at age 8, with polypectomy or surgical referral if polyps are numerous. Female patients require annual screenings for breast, uterine, ovarian, and cervical cancer.
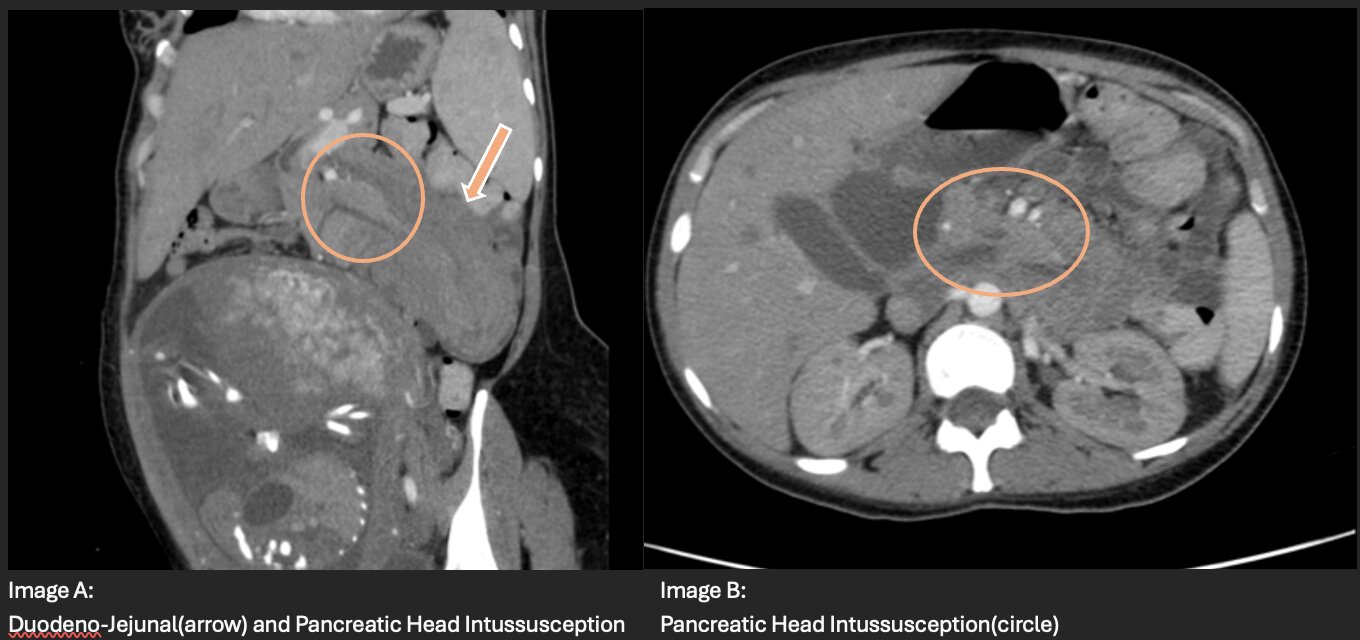
Figure: Duodenal, Jejunal and Pancreatic Head Intussusception
Disclosures:
Manuel Del Rio-Montesinos indicated no relevant financial relationships.
Viviana Blanco indicated no relevant financial relationships.
Pablo Costas indicated no relevant financial relationships.
Joan Neptune-Rosa indicated no relevant financial relationships.
Manuel Del Rio-Montesinos, MD1, Viviana Blanco, MD2, Pablo Costas, MD3, Joan Neptune-Rosa, BS4. P1796 - Untangled Mystery: Peutz-Jeghers Syndrome Unmasked by Pancreatic Intussusception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

