Monday Poster Session
Category: Biliary/Pancreas
P1798 - Duodenal Perforation Secondary to Biliary Stent Migration After ERCP for Periampullary Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdellatif Ismail, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Monzer Abdalla, MD1, Bidhisa Kharel, MBBS1, Shamsa Abdelatif, MBBS2, Abdellatif Ismail, MD3, Tarek Aboursheid, MD1, Natchaya Polpichai, MD4, Binayak Upadhyay, MD5, Amit Patel, MD6
1Ascension Saint Francis Hospital, Evanston, IL; 2University of Medical Sciences and Technology, Evanston, IL; 3University of Maryland Medical Center, Baltimore, MD; 4Weiss Memorial Hospital, Chicago, IL; 5University of Kentucky, Lexington, KY; 6GI Alliance of Illinois, Chicago, IL
Introduction: Biliary stents have been widely used to manage biliary obstruction and leaks. Stent migration rarely occurs, but it usually passes without adverse events. There are rare occasions when stent migration can be complicated by bowel perforation. Herein, we report a case of duodenal perforation caused by a migrated plastic biliary stent.
Case Description/Methods: An 80-year-old female with a history of recently diagnosed periampullary adenocarcinoma presented to the hospital with a fever and shortness of breath. One week before this presentation, she was diagnosed with periampullary adenocarcinoma with liver metastases after she presented with features of obstructive jaundice and underwent ERCP with the placement of two stents, 10 Fr 7mm into the common bile duct and 10 Fr 15 mm into the right intrahepatic duct.
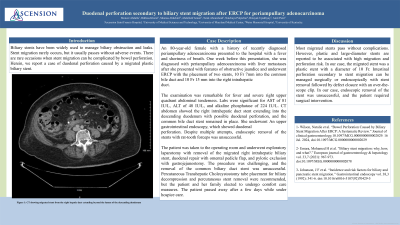
The examination was remarkable for fever and severe right upper quadrant abdominal tenderness. Labs were significant for AST of 81 IU/L, ALT of 48 IU/L, and alkaline phosphatase of 224 IU/L. CT abdomen showed the right intrahepatic duct stent extending into the descending duodenum with possible duodenal perforation, and the common bile duct stent remained in place. She underwent An upper gastrointestinal endoscopy, which showed duodenal perforation. Despite multiple attempts, endoscopic removal of the stents with rat-tooth forceps was unsuccessful.
The patient was taken to the operating room and underwent exploratory laparotomy with removal of the migrated right intrahepatic biliary stent, duodenal repair with omental pedicle flap, and pyloric exclusion with gastrojejunostomy. The procedure was challenging, and the removal of the common biliary duct stent was unsuccessful. Percutaneous Transhepatic Cholecystostomy tube placement for biliary decompression and percutaneous stent removal were recommended, but the patient and her family elected to undergo comfort care measures. The patient passed away after a few days while under hospice care.
Discussion: Most migrated stents pass without complications. However, plastic and large-diameter stents are reported to be associated with high migration and perforation risk. In our case, the migrated stent was a plastic stent with a diameter of 10 Fr. Intestinal perforation secondary to stent migration can be managed surgically or endoscopically with stent removal followed by defect closure with an over-the-scope clip. In our case, endoscopic removal of the stent was unsuccessful, and the patient required surgical intervention.
Disclosures:
Monzer Abdalla, MD1, Bidhisa Kharel, MBBS1, Shamsa Abdelatif, MBBS2, Abdellatif Ismail, MD3, Tarek Aboursheid, MD1, Natchaya Polpichai, MD4, Binayak Upadhyay, MD5, Amit Patel, MD6. P1798 - Duodenal Perforation Secondary to Biliary Stent Migration After ERCP for Periampullary Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Saint Francis Hospital, Evanston, IL; 2University of Medical Sciences and Technology, Evanston, IL; 3University of Maryland Medical Center, Baltimore, MD; 4Weiss Memorial Hospital, Chicago, IL; 5University of Kentucky, Lexington, KY; 6GI Alliance of Illinois, Chicago, IL
Introduction: Biliary stents have been widely used to manage biliary obstruction and leaks. Stent migration rarely occurs, but it usually passes without adverse events. There are rare occasions when stent migration can be complicated by bowel perforation. Herein, we report a case of duodenal perforation caused by a migrated plastic biliary stent.
Case Description/Methods: An 80-year-old female with a history of recently diagnosed periampullary adenocarcinoma presented to the hospital with a fever and shortness of breath. One week before this presentation, she was diagnosed with periampullary adenocarcinoma with liver metastases after she presented with features of obstructive jaundice and underwent ERCP with the placement of two stents, 10 Fr 7mm into the common bile duct and 10 Fr 15 mm into the right intrahepatic duct.
The examination was remarkable for fever and severe right upper quadrant abdominal tenderness. Labs were significant for AST of 81 IU/L, ALT of 48 IU/L, and alkaline phosphatase of 224 IU/L. CT abdomen showed the right intrahepatic duct stent extending into the descending duodenum with possible duodenal perforation, and the common bile duct stent remained in place. She underwent An upper gastrointestinal endoscopy, which showed duodenal perforation. Despite multiple attempts, endoscopic removal of the stents with rat-tooth forceps was unsuccessful.
The patient was taken to the operating room and underwent exploratory laparotomy with removal of the migrated right intrahepatic biliary stent, duodenal repair with omental pedicle flap, and pyloric exclusion with gastrojejunostomy. The procedure was challenging, and the removal of the common biliary duct stent was unsuccessful. Percutaneous Transhepatic Cholecystostomy tube placement for biliary decompression and percutaneous stent removal were recommended, but the patient and her family elected to undergo comfort care measures. The patient passed away after a few days while under hospice care.
Discussion: Most migrated stents pass without complications. However, plastic and large-diameter stents are reported to be associated with high migration and perforation risk. In our case, the migrated stent was a plastic stent with a diameter of 10 Fr. Intestinal perforation secondary to stent migration can be managed surgically or endoscopically with stent removal followed by defect closure with an over-the-scope clip. In our case, endoscopic removal of the stent was unsuccessful, and the patient required surgical intervention.
Disclosures:
Monzer Abdalla indicated no relevant financial relationships.
Bidhisa Kharel indicated no relevant financial relationships.
Shamsa Abdelatif indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Tarek Aboursheid indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Binayak Upadhyay indicated no relevant financial relationships.
Amit Patel indicated no relevant financial relationships.
Monzer Abdalla, MD1, Bidhisa Kharel, MBBS1, Shamsa Abdelatif, MBBS2, Abdellatif Ismail, MD3, Tarek Aboursheid, MD1, Natchaya Polpichai, MD4, Binayak Upadhyay, MD5, Amit Patel, MD6. P1798 - Duodenal Perforation Secondary to Biliary Stent Migration After ERCP for Periampullary Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
