Sunday Poster Session
Category: Stomach
P1700 - Metastatic Amelanotic Melanoma to the Stomach: A Rare Case
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Thaddeus Sullivan, DO
Arnot Ogden Medical Center
Clinton, NY
Presenting Author(s)
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Saeed Zaman, MD3, Tenzin Tseky, DO4, Gary Valvano, DO4
1Arnot Ogden Medical Center, Clinton, NY; 2Digestive Disease Medicine, New Hartford, NY; 3Digestive Disease Medicine, Utica, NY; 4Arnot Ogden Medical Center, Elmira, NY
Introduction: While malignant melanoma is an extraordinarily rare cause for metastatic involvement of the stomach, it is one of the more common etiologies of metastatic involvement of the stomach. This particular case is extraordinarily singular as no primary was ever identified. The patient is presumed to have amelanotic melanoma.
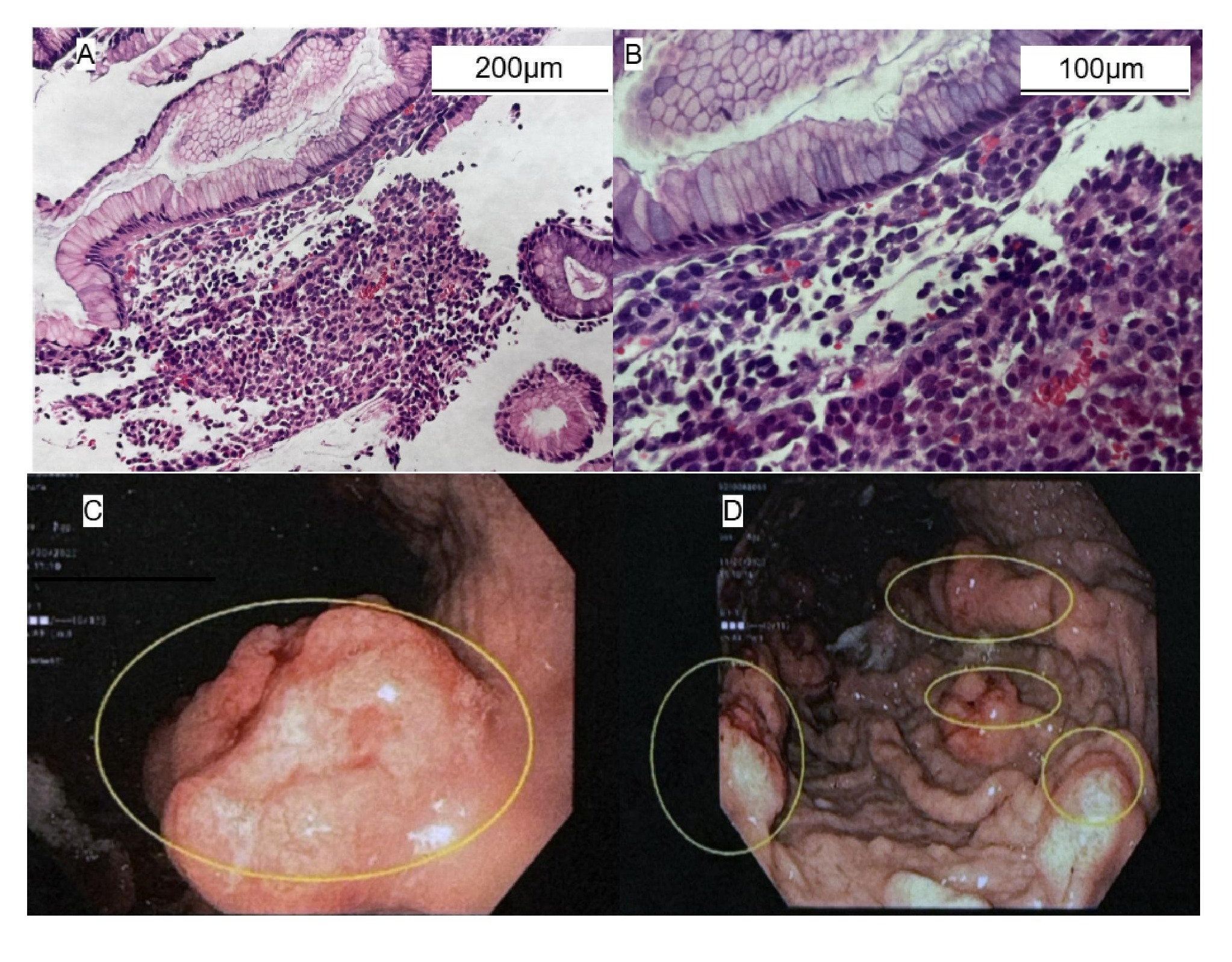
Case Description/Methods: A 72-year-old male with a history of malignant melanoma in situ of the scalp 22 years earlier presented with a two-month history of reflux symptoms, early satiety and 30 pounds of weight loss. He has no history of invasive malignant melanoma. CBC showed hemoglobin was 12.7, hematocrit 39.9, MCV 88 and stool was guaiac negative. He also had diarrhea with 2-3 loose stools per day during that time span. Upper endoscopy revealed multiple inflammatory friable gastric lesions. Biopsy confirmed metastatic malignant melanoma. Subsequent diagnostic imaging revealed metastatic involvement of porta hepatis. He was not a candidate for palliative surgery. A thorough physical exam revealed no evidence of a primary. We concluded that the patient had amelanotic melanoma.
Discussion: Though metastatic disease to the stomach is extremely rare, metastatic melanoma must be considered. Involvement of the stomach has been reported to be 0.2-1.7%. Malignant melanoma has been reported as the most common primary malignancy with metastatic involvement of the stomach. Using endoscopy appearance to characterize metastatic lesions of the stomach, two thirds of these patients have mucosal lesions while one third have submucosal lesions, as seen in this patient. Typically, patients present with epigastric pain, nausea, vomiting, iron deficiency anemia and guaiac positive stool. This patient did not have microcytic anemia or guaiac positive stool. Risk factors for malignant melanoma include family history, phenotypic traits, and prior history of malignant melanoma. This patient had malignant melanoma 22 years earlier. It is felt that particular lesion did not contribute to this patient's metastatic disease. The four main subtypes of cutaneous melanoma are superficial spreading, nodular, lentigo maligna, and acral lentiginous. 8% of patients with melanoma have amelanotic melanoma in which the melanoma tumor cells are no longer manufacturing pigment. This is not readily recognized. Patients with solitary metastatic involvement may be considered for palliative wedge resection. This patient had multiple lesions in the stomach and was not considered to be a surgical candidate.
Disclosures:
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Saeed Zaman, MD3, Tenzin Tseky, DO4, Gary Valvano, DO4. P1700 - Metastatic Amelanotic Melanoma to the Stomach: A Rare Case, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Arnot Ogden Medical Center, Clinton, NY; 2Digestive Disease Medicine, New Hartford, NY; 3Digestive Disease Medicine, Utica, NY; 4Arnot Ogden Medical Center, Elmira, NY
Introduction: While malignant melanoma is an extraordinarily rare cause for metastatic involvement of the stomach, it is one of the more common etiologies of metastatic involvement of the stomach. This particular case is extraordinarily singular as no primary was ever identified. The patient is presumed to have amelanotic melanoma.
Case Description/Methods: A 72-year-old male with a history of malignant melanoma in situ of the scalp 22 years earlier presented with a two-month history of reflux symptoms, early satiety and 30 pounds of weight loss. He has no history of invasive malignant melanoma. CBC showed hemoglobin was 12.7, hematocrit 39.9, MCV 88 and stool was guaiac negative. He also had diarrhea with 2-3 loose stools per day during that time span. Upper endoscopy revealed multiple inflammatory friable gastric lesions. Biopsy confirmed metastatic malignant melanoma. Subsequent diagnostic imaging revealed metastatic involvement of porta hepatis. He was not a candidate for palliative surgery. A thorough physical exam revealed no evidence of a primary. We concluded that the patient had amelanotic melanoma.
Discussion: Though metastatic disease to the stomach is extremely rare, metastatic melanoma must be considered. Involvement of the stomach has been reported to be 0.2-1.7%. Malignant melanoma has been reported as the most common primary malignancy with metastatic involvement of the stomach. Using endoscopy appearance to characterize metastatic lesions of the stomach, two thirds of these patients have mucosal lesions while one third have submucosal lesions, as seen in this patient. Typically, patients present with epigastric pain, nausea, vomiting, iron deficiency anemia and guaiac positive stool. This patient did not have microcytic anemia or guaiac positive stool. Risk factors for malignant melanoma include family history, phenotypic traits, and prior history of malignant melanoma. This patient had malignant melanoma 22 years earlier. It is felt that particular lesion did not contribute to this patient's metastatic disease. The four main subtypes of cutaneous melanoma are superficial spreading, nodular, lentigo maligna, and acral lentiginous. 8% of patients with melanoma have amelanotic melanoma in which the melanoma tumor cells are no longer manufacturing pigment. This is not readily recognized. Patients with solitary metastatic involvement may be considered for palliative wedge resection. This patient had multiple lesions in the stomach and was not considered to be a surgical candidate.
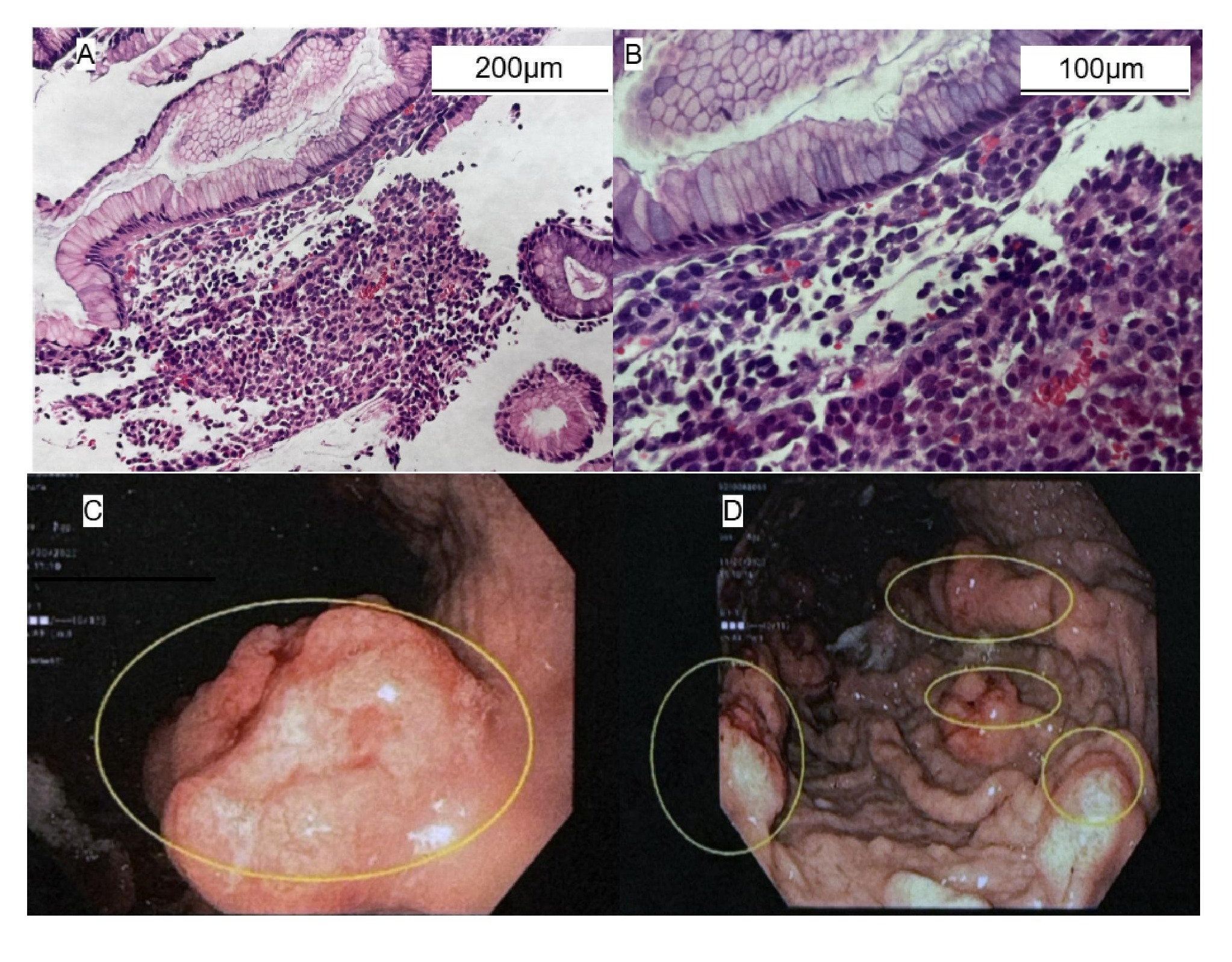
Figure: A,B- Hematoxylin and eosin stain, melanocytes are demonstrated in submucosal position. Mucosa is not violated.
C- Gastric body/cardia polyploid lesion
D-Gastric body multiple polyploid lesions
C- Gastric body/cardia polyploid lesion
D-Gastric body multiple polyploid lesions
Disclosures:
Thaddeus Sullivan indicated no relevant financial relationships.
Bradley Sklar indicated no relevant financial relationships.
Saeed Zaman indicated no relevant financial relationships.
Tenzin Tseky indicated no relevant financial relationships.
Gary Valvano indicated no relevant financial relationships.
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Saeed Zaman, MD3, Tenzin Tseky, DO4, Gary Valvano, DO4. P1700 - Metastatic Amelanotic Melanoma to the Stomach: A Rare Case, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
