Monday Poster Session
Category: Biliary/Pancreas
P1714 - Trends in Mortality Due to Pancreatitis Among Patients Aged 55 and Older in the United States: Insights from the CDC WONDER Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Amira Al-Nabolsi, DO
Corewell Health Farmington Hills
Dearborn, MI
Presenting Author(s)
Ammad Javaid. Chaudhary, MD1, Amira Al-Nabolsi, DO2, Muhammad Naveed, MBBS3, Ahila Ali, MBBS3, Rabia Iqbal, MBBS3, Bazil Azeem, MBBS4, Muhammad Omer Rehan, MBBS3, Rabia Asim, MBBS5, Nouman Shafique, MD6, Syed-Mohammed Jafri, MD1, Faiza Ashfaque, MBBS3
1Henry Ford Health, Detroit, MI; 2Corewell Health Farmington Hills, Dearborn, MI; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Shaheed Mohtarma Benazir Bhutto Medical College, Karachi, Sindh, Pakistan; 5Mohtarma Benazir Bhutto Medical College, Karachi, Sindh, Pakistan; 6AdventHealth Medical Group, AdventHealth, Orlando, FL
Introduction: Pancreatitis remains one of the leading causes of death in the elderly in the United States. This study intents to analyze trends and demographic differences in mortality due to pancreatitis among patients aged 55 and older from 1999 to 2020.
Methods: We employed a retrospective analysis to calculate age-adjusted mortality rates (AAMRs) per 100,000 persons using data from the CDC WONDER database. Average Annual Percentage Change (AAPC) and Annual Percentage Change (APC) were used to estimate the trends by calendar year, sex, race/ethnicity and geographic region.
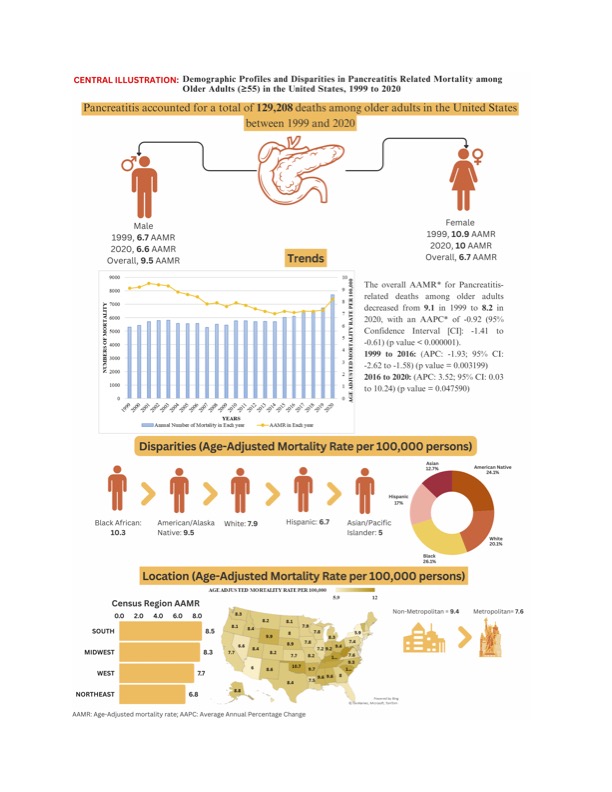
Results: Between 1999 and 2020, pancreatitis caused 129,208 deaths among older U.S. adults (55+). Most fatalities occurred in medical facilities (68.1%). The overall AAMR for pancreatitis-related deaths decreased from 9.1 in 1999 to 8.2 in 2020, with an AAPC of -0.92 (95% CI: -1.41 to -0.61, p < 0.000001). A moderate decline was seen from 1999 to 2016 (APC: -1.93, p = 0.003199), followed by a sharper increase from 2016 to 2020 (APC: 3.52, p = 0.047590). Stratified by sex, older men had higher AAMRs compared to older women (men: 9.5; women: 6.7). Both genders saw decreased AAMRs, with a slightly more pronounced decrease in women (men: AAPC: -0.91, p < 0.000001; women: AAPC: -1.01, p < 0.000001). Racial disparities were evident, with the highest number of deaths among Whites (78.90%). AAMRs were highest among Black or African Americans, followed by American Indians or Alaska Natives, Whites, Hispanics, and Asians. All racial groups saw variable decreases in AAMRs from 1999 to 2020, with the most pronounced decline in Asians (AAPC: -3.36, p < 0.000001). Geographically, AAMRs varied, highest in West Virginia (12) and lowest in New York (5.9). The Southern region had the highest average mortality (8.5). Nonmetropolitan areas had higher AAMRs than metropolitan areas (9.4 vs. 7.6). Both areas saw decreases in AAMRs from 1999 to 2020.
Discussion: This study identifies trends and disparities in pancreatitis mortality among older adults in the US. Despite declining overall rates, differences persist across sex, race/ethnicity, and regions. Targeted interventions and equitable healthcare access are crucial to reduce mortality and enhance outcomes. Further research is needed to understand and address these disparities effectively.
Disclosures:
Ammad Javaid. Chaudhary, MD1, Amira Al-Nabolsi, DO2, Muhammad Naveed, MBBS3, Ahila Ali, MBBS3, Rabia Iqbal, MBBS3, Bazil Azeem, MBBS4, Muhammad Omer Rehan, MBBS3, Rabia Asim, MBBS5, Nouman Shafique, MD6, Syed-Mohammed Jafri, MD1, Faiza Ashfaque, MBBS3. P1714 - Trends in Mortality Due to Pancreatitis Among Patients Aged 55 and Older in the United States: Insights from the CDC WONDER Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Corewell Health Farmington Hills, Dearborn, MI; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Shaheed Mohtarma Benazir Bhutto Medical College, Karachi, Sindh, Pakistan; 5Mohtarma Benazir Bhutto Medical College, Karachi, Sindh, Pakistan; 6AdventHealth Medical Group, AdventHealth, Orlando, FL
Introduction: Pancreatitis remains one of the leading causes of death in the elderly in the United States. This study intents to analyze trends and demographic differences in mortality due to pancreatitis among patients aged 55 and older from 1999 to 2020.
Methods: We employed a retrospective analysis to calculate age-adjusted mortality rates (AAMRs) per 100,000 persons using data from the CDC WONDER database. Average Annual Percentage Change (AAPC) and Annual Percentage Change (APC) were used to estimate the trends by calendar year, sex, race/ethnicity and geographic region.
Results: Between 1999 and 2020, pancreatitis caused 129,208 deaths among older U.S. adults (55+). Most fatalities occurred in medical facilities (68.1%). The overall AAMR for pancreatitis-related deaths decreased from 9.1 in 1999 to 8.2 in 2020, with an AAPC of -0.92 (95% CI: -1.41 to -0.61, p < 0.000001). A moderate decline was seen from 1999 to 2016 (APC: -1.93, p = 0.003199), followed by a sharper increase from 2016 to 2020 (APC: 3.52, p = 0.047590). Stratified by sex, older men had higher AAMRs compared to older women (men: 9.5; women: 6.7). Both genders saw decreased AAMRs, with a slightly more pronounced decrease in women (men: AAPC: -0.91, p < 0.000001; women: AAPC: -1.01, p < 0.000001). Racial disparities were evident, with the highest number of deaths among Whites (78.90%). AAMRs were highest among Black or African Americans, followed by American Indians or Alaska Natives, Whites, Hispanics, and Asians. All racial groups saw variable decreases in AAMRs from 1999 to 2020, with the most pronounced decline in Asians (AAPC: -3.36, p < 0.000001). Geographically, AAMRs varied, highest in West Virginia (12) and lowest in New York (5.9). The Southern region had the highest average mortality (8.5). Nonmetropolitan areas had higher AAMRs than metropolitan areas (9.4 vs. 7.6). Both areas saw decreases in AAMRs from 1999 to 2020.
Discussion: This study identifies trends and disparities in pancreatitis mortality among older adults in the US. Despite declining overall rates, differences persist across sex, race/ethnicity, and regions. Targeted interventions and equitable healthcare access are crucial to reduce mortality and enhance outcomes. Further research is needed to understand and address these disparities effectively.
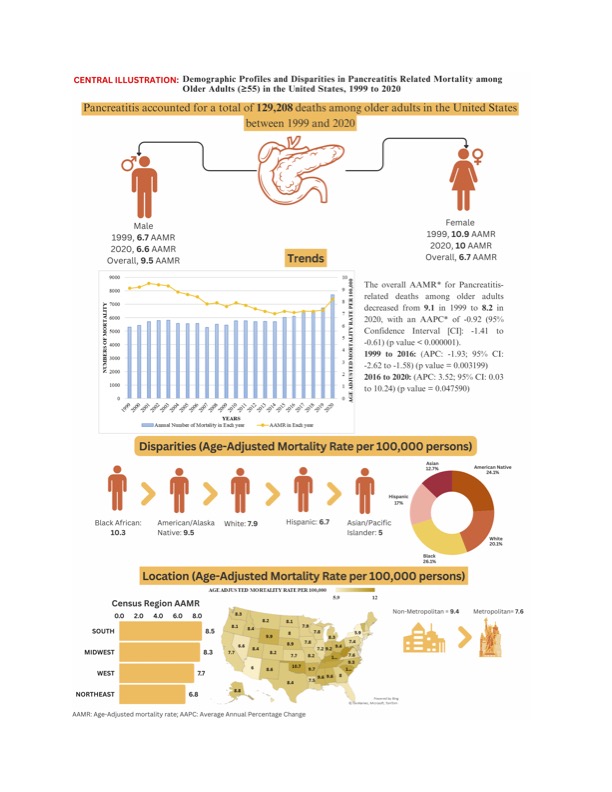
Figure: Pancreatitis Profiles and Disparities in Pancreatitis Related Mortality Among Older Adults (>55) in the United States, 1999 to 2020
Disclosures:
Ammad Chaudhary indicated no relevant financial relationships.
Amira Al-Nabolsi indicated no relevant financial relationships.
Muhammad Naveed indicated no relevant financial relationships.
Ahila Ali indicated no relevant financial relationships.
Rabia Iqbal indicated no relevant financial relationships.
Bazil Azeem indicated no relevant financial relationships.
Muhammad Omer Rehan indicated no relevant financial relationships.
Rabia Asim indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie, Intercept, VectivBio – Advisor or Review Panel Member, Speakers Bureau.
Faiza Ashfaque indicated no relevant financial relationships.
Ammad Javaid. Chaudhary, MD1, Amira Al-Nabolsi, DO2, Muhammad Naveed, MBBS3, Ahila Ali, MBBS3, Rabia Iqbal, MBBS3, Bazil Azeem, MBBS4, Muhammad Omer Rehan, MBBS3, Rabia Asim, MBBS5, Nouman Shafique, MD6, Syed-Mohammed Jafri, MD1, Faiza Ashfaque, MBBS3. P1714 - Trends in Mortality Due to Pancreatitis Among Patients Aged 55 and Older in the United States: Insights from the CDC WONDER Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

