Sunday Poster Session
Category: Stomach
P1622 - Evaluating Prophylactic Gastric Acid Suppression and Risk Factors for Gastrointestinal Adverse Effects in Chronic NSAID Users: A Retrospective Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Alexander Garcia, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Alexander Garcia, DO1, Avneet Singh, DO1, Nicole Melchiorre, BS2, Emily Serata, BS2, Fariha Hasan, MD3, Lucinda Lau, BS2, Mary Penckofer, BS2, Joseph Sichel, BS2, Krystal Hunter, PhD, MBA4, Shikha Talwar, MD5, Satyajeet Roy, MD1
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Hospital, Philadelphia, PA; 4Cooper University Health Care, Camden, NJ; 5Einstein Healthcare Network, Philadelphia, PA
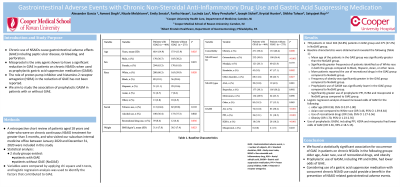
Introduction: Chronic use of non-steroidal anti-inflammatory drugs (NSAIDs) causes gastrointestinal adverse effects (GIAE), such as peptic ulcer disease (25-50%), gastrointestinal bleeding (2-4%), and perforation. In the outpatient setting, data has shown varying results regarding the use of prophylactic gastric acid suppression medication (GASM) in patients using chronic NSAIDs. We aim to study the association of prophylactic GASM in patients with or without GIAE.
Methods: We performed a retrospective review of patients aged 18 years and older, on chronic NSAID treatment for greater than 3 months who visited a suburban internal medicine office between January 1, 2020 and December 31, 2020. Two study groups were identified, patients with GIAE and those without (NoGIAE). Variables were compared by applying chi square and t-tests, and logistic regression analysis was used to identify the factors that contributed to GIAE.
Results: Among 739 patients reviewed, there were 464 (62.8 %) patients in the GIAE group and 275 (37.2 %) in NoGIAE group. The mean age in the GAIE group was significantly greater than the NoGAIE group (60.4 +/-14.9 vs 57.9 +/-13.9 years; P=0.025). There were significantly greater frequencies of patients identified as of White race (60.3 % and 59.9 %) in both the GIAE and NoGIAE groups compared to Black, Hispanic, Asian, or other races (19.1%, 11.1 %, 6.7 %, 2.8 % and 59.9 %, 20.4 %, 10.6 %, 2.6 %, 6.5 %; P=0.020). Logistic regression analysis showed decreased odds of GIAE for older age (OR 0.98, 95 % CI 0.972-0.995; p=.004) and increased odds with obesity (OR 1.70, 95 % CI 1.23-2.35; P=.001), Asian race compared to White (OR 3.46, 95 % CI 1.39-8.64; P=.008) and use of recreational drugs (OR 2.66, 95 % CI 1.27-5.56; p=.009). Prophylactic use of all GASM was significantly lower in the GIAE group compared to the NoGIAE group (16.0 % vs 30.2 %; P< 0.001). There was significantly greater use of prophylactic PPI and H2RA in the NoGIAE group compared to the GIAE group (18.5 %, 10.2 % vs 12.1 %, 3.9 %; P< 0.001). Patients without prophylactic GASM, including PPI, H2RA, and misoprostol had higher odds of GAIE (OR 3.36, 95 % 2.18-5.15).
Discussion: This retrospective study suggests that caution should be utilized in the chronic prescribing of NSAIDs in specific patient populations that may be at increased risk for GIAE. In addition, we propose the importance of considering GASM, specifically PPI or H2RAs, with the long-term use of NSAIDs to prevent GIAE.
Disclosures:
Alexander Garcia, DO1, Avneet Singh, DO1, Nicole Melchiorre, BS2, Emily Serata, BS2, Fariha Hasan, MD3, Lucinda Lau, BS2, Mary Penckofer, BS2, Joseph Sichel, BS2, Krystal Hunter, PhD, MBA4, Shikha Talwar, MD5, Satyajeet Roy, MD1. P1622 - Evaluating Prophylactic Gastric Acid Suppression and Risk Factors for Gastrointestinal Adverse Effects in Chronic NSAID Users: A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Hospital, Philadelphia, PA; 4Cooper University Health Care, Camden, NJ; 5Einstein Healthcare Network, Philadelphia, PA
Introduction: Chronic use of non-steroidal anti-inflammatory drugs (NSAIDs) causes gastrointestinal adverse effects (GIAE), such as peptic ulcer disease (25-50%), gastrointestinal bleeding (2-4%), and perforation. In the outpatient setting, data has shown varying results regarding the use of prophylactic gastric acid suppression medication (GASM) in patients using chronic NSAIDs. We aim to study the association of prophylactic GASM in patients with or without GIAE.
Methods: We performed a retrospective review of patients aged 18 years and older, on chronic NSAID treatment for greater than 3 months who visited a suburban internal medicine office between January 1, 2020 and December 31, 2020. Two study groups were identified, patients with GIAE and those without (NoGIAE). Variables were compared by applying chi square and t-tests, and logistic regression analysis was used to identify the factors that contributed to GIAE.
Results: Among 739 patients reviewed, there were 464 (62.8 %) patients in the GIAE group and 275 (37.2 %) in NoGIAE group. The mean age in the GAIE group was significantly greater than the NoGAIE group (60.4 +/-14.9 vs 57.9 +/-13.9 years; P=0.025). There were significantly greater frequencies of patients identified as of White race (60.3 % and 59.9 %) in both the GIAE and NoGIAE groups compared to Black, Hispanic, Asian, or other races (19.1%, 11.1 %, 6.7 %, 2.8 % and 59.9 %, 20.4 %, 10.6 %, 2.6 %, 6.5 %; P=0.020). Logistic regression analysis showed decreased odds of GIAE for older age (OR 0.98, 95 % CI 0.972-0.995; p=.004) and increased odds with obesity (OR 1.70, 95 % CI 1.23-2.35; P=.001), Asian race compared to White (OR 3.46, 95 % CI 1.39-8.64; P=.008) and use of recreational drugs (OR 2.66, 95 % CI 1.27-5.56; p=.009). Prophylactic use of all GASM was significantly lower in the GIAE group compared to the NoGIAE group (16.0 % vs 30.2 %; P< 0.001). There was significantly greater use of prophylactic PPI and H2RA in the NoGIAE group compared to the GIAE group (18.5 %, 10.2 % vs 12.1 %, 3.9 %; P< 0.001). Patients without prophylactic GASM, including PPI, H2RA, and misoprostol had higher odds of GAIE (OR 3.36, 95 % 2.18-5.15).
Discussion: This retrospective study suggests that caution should be utilized in the chronic prescribing of NSAIDs in specific patient populations that may be at increased risk for GIAE. In addition, we propose the importance of considering GASM, specifically PPI or H2RAs, with the long-term use of NSAIDs to prevent GIAE.
Disclosures:
Alexander Garcia indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Nicole Melchiorre indicated no relevant financial relationships.
Emily Serata indicated no relevant financial relationships.
Fariha Hasan indicated no relevant financial relationships.
Lucinda Lau indicated no relevant financial relationships.
Mary Penckofer indicated no relevant financial relationships.
Joseph Sichel indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Shikha Talwar indicated no relevant financial relationships.
Satyajeet Roy indicated no relevant financial relationships.
Alexander Garcia, DO1, Avneet Singh, DO1, Nicole Melchiorre, BS2, Emily Serata, BS2, Fariha Hasan, MD3, Lucinda Lau, BS2, Mary Penckofer, BS2, Joseph Sichel, BS2, Krystal Hunter, PhD, MBA4, Shikha Talwar, MD5, Satyajeet Roy, MD1. P1622 - Evaluating Prophylactic Gastric Acid Suppression and Risk Factors for Gastrointestinal Adverse Effects in Chronic NSAID Users: A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
