Sunday Poster Session
Category: Stomach
P1625 - Ectopic Pancreatic Mass Inducing Gastric Outlet Obstruction
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohan Ahuja, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Rohan Ahuja, MD1, Nakia Armendariz, BS1, Nitish Mittal, MD1, Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Kazi T. Haque, MD2, Jimmy Pham, MD1, Madhav Desai, MD3
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health, McGovern Medical School, Pearland, TX; 3University of Texas Health Science Center, Houston, TX
Introduction: Gastric outlet obstruction (GOO) is a clinical diagnosis characterized by early satiety, abdominal pain, post-prandial vomiting, and weight loss. Three categories of obstruction include benign, malignant, and gastroparesis-induced GOO. Amongst benign causes, GOO can occur due to medication use, toxic ingestion, anatomical obstruction, or inflammatory conditions. Perigastric cysts are a more infrequent cause of anatomical GOO. Here, we present the rare case of an ectopic pancreatic cyst-inducing GOO highlighting the importance of a thorough diagnostic workup.
Case Description/Methods: A 40-year-old man with no prior past medical or surgical history presented with 6 months of intermittent epigastric pain, nausea, and vomiting with an inability to tolerate oral intake for a week. Laboratory evaluation was only notable for a leukocytosis of 18.2. However, CT abdomen and pelvis revealed a 4.5 x 3.0 x 2.9 cm well-circumscribed peripherally enhancing cystic lesion in the distal pylorus. Initial esophagogastroduodenoscopy (EGD) revealed an obstructive submucosal mass at the antrum. Random gastric biopsies were negative for malignancy or evidence of H. pylori. Endoscopic ultrasound was performed upon repeat EGD for further characterization of the submucosal lesion, revealing a 5 cm x 5 cm perigastric cyst with anechoic and hypoechoic areas at the site of extrinsic compression in the gastric antrum. Pancreas visualization revealed sequelae of chronic pancreatitis with hyperechoic stranding. Under doppler guidance, fine needle aspiration was performed with dark brown aspirate and pyloric narrowing resolution due to cyst size reduction. Subsequently, the patient’s symptoms significantly improved. Fluid analysis sent from aspirate revealed an elevated CEA level at 736 ng/mL and amylase of 2113 ng/m, indicating the nature of the cystic lesion to be ectopic mucinous pancreatic tissue.
Discussion: Ectopic pancreas most commonly is in the antrum and is typically asymptomatic. This is a rare case of ectopic pancreatic mass leading to GOO. It is unclear the mechanism of growth of the cyst but could be explained by continuous mucinous secretions given the elevated CEA or evidence of chronic pancreatitis on EUS leading to continuous extravasation. Few case reports exist in the current literature with EUS performed most often for diagnostic and therapeutic evaluation. In conclusion, ectopic pancreas should be a consideration in clinicians’ differential diagnosis when evaluating patients for GOO.
Disclosures:
Rohan Ahuja, MD1, Nakia Armendariz, BS1, Nitish Mittal, MD1, Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Kazi T. Haque, MD2, Jimmy Pham, MD1, Madhav Desai, MD3. P1625 - Ectopic Pancreatic Mass Inducing Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health, McGovern Medical School, Pearland, TX; 3University of Texas Health Science Center, Houston, TX
Introduction: Gastric outlet obstruction (GOO) is a clinical diagnosis characterized by early satiety, abdominal pain, post-prandial vomiting, and weight loss. Three categories of obstruction include benign, malignant, and gastroparesis-induced GOO. Amongst benign causes, GOO can occur due to medication use, toxic ingestion, anatomical obstruction, or inflammatory conditions. Perigastric cysts are a more infrequent cause of anatomical GOO. Here, we present the rare case of an ectopic pancreatic cyst-inducing GOO highlighting the importance of a thorough diagnostic workup.
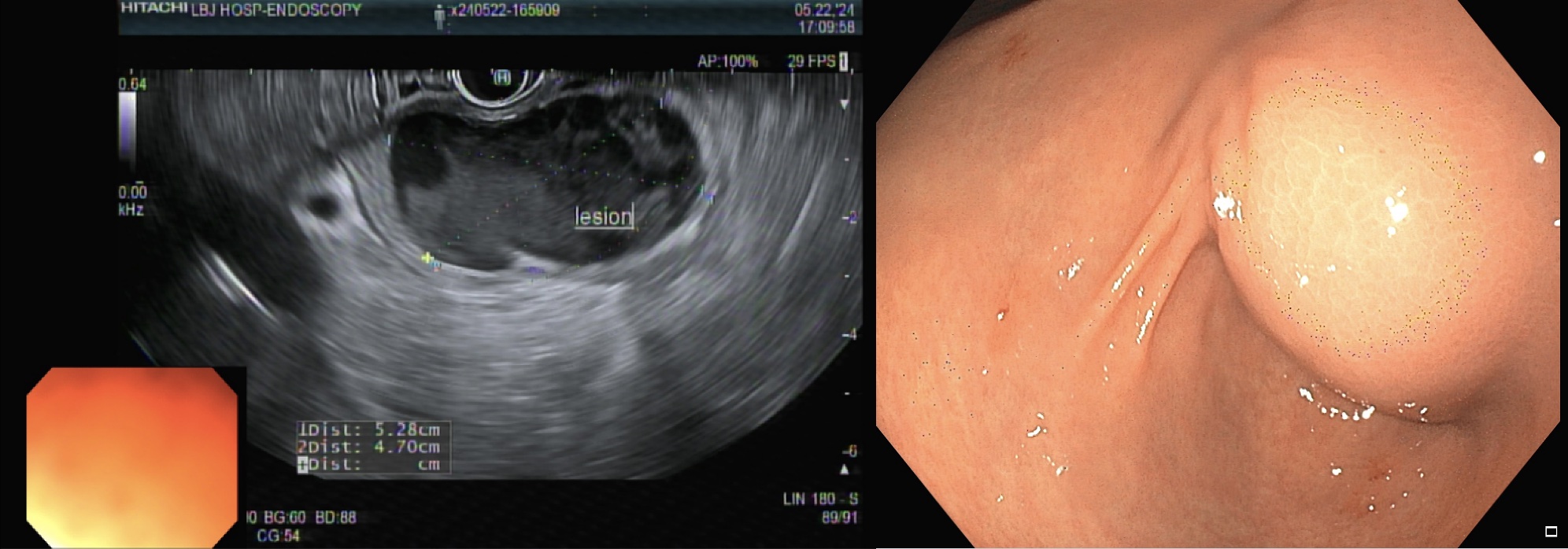
Case Description/Methods: A 40-year-old man with no prior past medical or surgical history presented with 6 months of intermittent epigastric pain, nausea, and vomiting with an inability to tolerate oral intake for a week. Laboratory evaluation was only notable for a leukocytosis of 18.2. However, CT abdomen and pelvis revealed a 4.5 x 3.0 x 2.9 cm well-circumscribed peripherally enhancing cystic lesion in the distal pylorus. Initial esophagogastroduodenoscopy (EGD) revealed an obstructive submucosal mass at the antrum. Random gastric biopsies were negative for malignancy or evidence of H. pylori. Endoscopic ultrasound was performed upon repeat EGD for further characterization of the submucosal lesion, revealing a 5 cm x 5 cm perigastric cyst with anechoic and hypoechoic areas at the site of extrinsic compression in the gastric antrum. Pancreas visualization revealed sequelae of chronic pancreatitis with hyperechoic stranding. Under doppler guidance, fine needle aspiration was performed with dark brown aspirate and pyloric narrowing resolution due to cyst size reduction. Subsequently, the patient’s symptoms significantly improved. Fluid analysis sent from aspirate revealed an elevated CEA level at 736 ng/mL and amylase of 2113 ng/m, indicating the nature of the cystic lesion to be ectopic mucinous pancreatic tissue.
Discussion: Ectopic pancreas most commonly is in the antrum and is typically asymptomatic. This is a rare case of ectopic pancreatic mass leading to GOO. It is unclear the mechanism of growth of the cyst but could be explained by continuous mucinous secretions given the elevated CEA or evidence of chronic pancreatitis on EUS leading to continuous extravasation. Few case reports exist in the current literature with EUS performed most often for diagnostic and therapeutic evaluation. In conclusion, ectopic pancreas should be a consideration in clinicians’ differential diagnosis when evaluating patients for GOO.
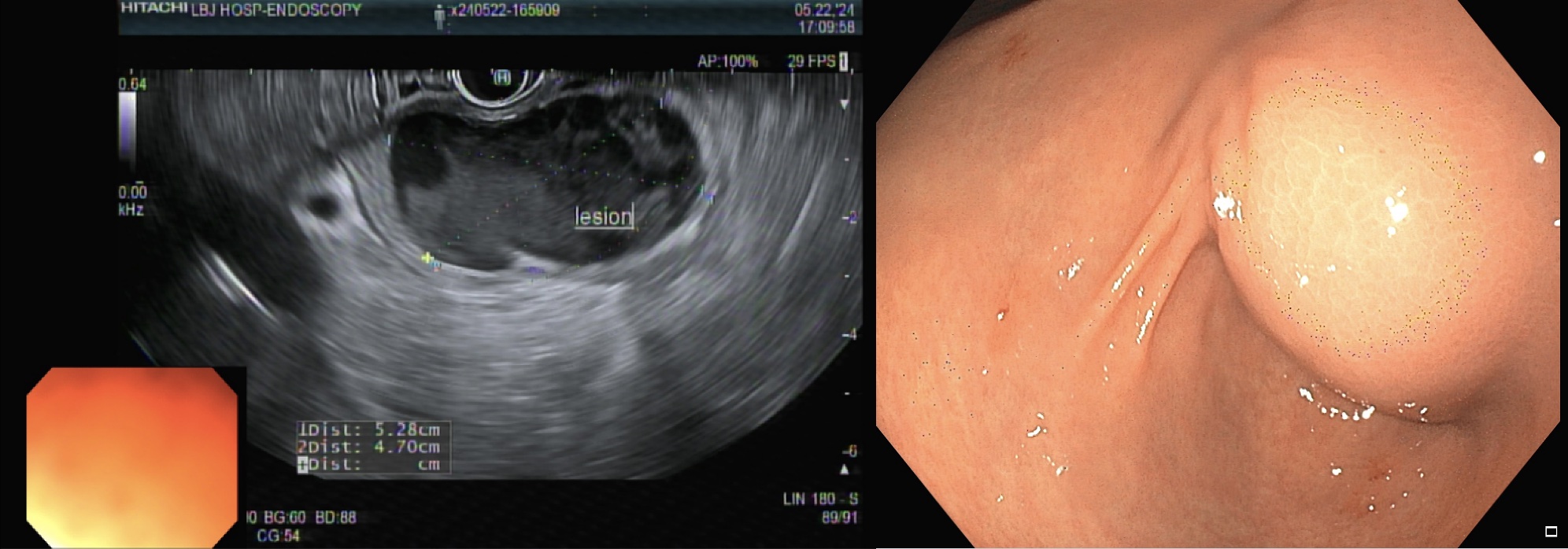
Figure: EUS and Endoscopic Visualization of Submucosal Pancreatic Mass
Disclosures:
Rohan Ahuja indicated no relevant financial relationships.
Nakia Armendariz indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Jimmy Pham indicated no relevant financial relationships.
Madhav Desai indicated no relevant financial relationships.
Rohan Ahuja, MD1, Nakia Armendariz, BS1, Nitish Mittal, MD1, Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Kazi T. Haque, MD2, Jimmy Pham, MD1, Madhav Desai, MD3. P1625 - Ectopic Pancreatic Mass Inducing Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
