Sunday Poster Session
Category: Small Intestine
P1552 - A “Fishy” Cause of Epigastric Pain
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JS
Julie Sullivan, DO
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Julie Sullivan, DO, Michael L. Davis, DO
Albert Einstein Medical Center, Philadelphia, PA
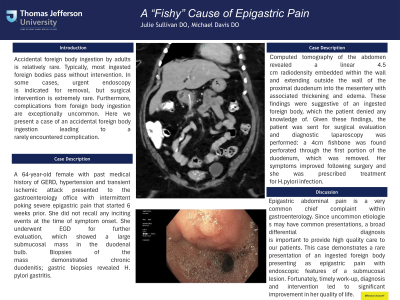
Introduction: Accidental foreign body ingestion by adults is relatively rare. Typically, most ingested foreign bodies pass without intervention. In some cases, urgent endoscopy is indicated for removal, but surgical intervention is extremely rare. Furthermore, complications from foreign body ingestion are exceptionally uncommon. Here we present a case of an accidental foreign body ingestion leading to a rarely encountered complication.
Case Description/Methods: A 64-year-old female with past medical history of GERD, hypertension and transient ischemic attack presented to the gastroenterology office with intermittent poking severe epigastric pain that started 6 weeks prior. She did not recall any inciting events at the time of symptom onset. She underwent EGD for further evaluation, which showed a large submucosal mass in the duodenal bulb. Biopsies of the mass demonstrated chronic duodenitis; gastric biopsies revealed H. pylori gastritis. Computed tomography of the abdomen revealed a linear 4.5 cm radiodensity embedded within the wall and extending outside the wall of the proximal duodenum into the mesentery with associated thickening and edema. These findings were suggestive of an ingested foreign body, which the patient denied any knowledge of. Given these findings, the patient was sent for surgical evaluation and diagnostic laparoscopy was performed: a 4cm fishbone was found perforated through the first portion of the duodenum, which was removed. Her symptoms improved following surgery and she was prescribed treatment for H.pylori infection.
Discussion: Epigastric abdominal pain is a very common chief complaint within gastroenterology. Since uncommon etiologies may have common presentations, a broad differential diagnosis is important to provide high quality care to our patients. This case demonstrates a rare presentation of an ingested foreign body presenting as epigastric pain with endoscopic features of a submucosal lesion. Fortunately, timely work-up, diagnosis and intervention led to significant improvement in her quality of life.
Disclosures:
Julie Sullivan, DO, Michael L. Davis, DO. P1552 - A “Fishy” Cause of Epigastric Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Albert Einstein Medical Center, Philadelphia, PA
Introduction: Accidental foreign body ingestion by adults is relatively rare. Typically, most ingested foreign bodies pass without intervention. In some cases, urgent endoscopy is indicated for removal, but surgical intervention is extremely rare. Furthermore, complications from foreign body ingestion are exceptionally uncommon. Here we present a case of an accidental foreign body ingestion leading to a rarely encountered complication.
Case Description/Methods: A 64-year-old female with past medical history of GERD, hypertension and transient ischemic attack presented to the gastroenterology office with intermittent poking severe epigastric pain that started 6 weeks prior. She did not recall any inciting events at the time of symptom onset. She underwent EGD for further evaluation, which showed a large submucosal mass in the duodenal bulb. Biopsies of the mass demonstrated chronic duodenitis; gastric biopsies revealed H. pylori gastritis. Computed tomography of the abdomen revealed a linear 4.5 cm radiodensity embedded within the wall and extending outside the wall of the proximal duodenum into the mesentery with associated thickening and edema. These findings were suggestive of an ingested foreign body, which the patient denied any knowledge of. Given these findings, the patient was sent for surgical evaluation and diagnostic laparoscopy was performed: a 4cm fishbone was found perforated through the first portion of the duodenum, which was removed. Her symptoms improved following surgery and she was prescribed treatment for H.pylori infection.
Discussion: Epigastric abdominal pain is a very common chief complaint within gastroenterology. Since uncommon etiologies may have common presentations, a broad differential diagnosis is important to provide high quality care to our patients. This case demonstrates a rare presentation of an ingested foreign body presenting as epigastric pain with endoscopic features of a submucosal lesion. Fortunately, timely work-up, diagnosis and intervention led to significant improvement in her quality of life.
Disclosures:
Julie Sullivan indicated no relevant financial relationships.
Michael Davis indicated no relevant financial relationships.
Julie Sullivan, DO, Michael L. Davis, DO. P1552 - A “Fishy” Cause of Epigastric Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
