Sunday Poster Session
Category: Obesity
P1438 - Low Utilization of Nutrition Counselling Among Hospitalized US Patients with NAFLD – Insights from the National Inpatient Sample Database 2016-2020
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Oladimeji E. Oluaderounmu, MD
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Oladimeji E. Oluaderounmu, MD1, Bede N. Nriagu, MD, MPH1, Mirza Fawad Ahmed, MD1, Pushkar Kumar, MBBS, MD2, Nicole E. Villa, MD1, Sai Gautham Kanagala, MD1, Sarav Daid, MD2, Jennifer Harley, MD1
1NYC Health + Hospitals/Metropolitan, New York, NY; 2New York Medical College, New York, NY
Introduction: Non-alcoholic fatty liver disease (NAFLD), recently renamed metabolic dysfunction-associated liver disease (MASLD), is the leading cause of chronic liver disease in developed countries, with its prevalence and economic impact on the rise. The primary management strategy for NAFLD is lifestyle modification and weight loss. This study aims to evaluate the use of nutrition counseling services for patients diagnosed with NAFLD during hospitalizations over a five-year period
Methods: The National Inpatient Sample database (2016-2020) was analyzed to identify hospitalizations for patients aged 18 and older with a primary diagnosis of NAFLD. We further examined the subset of these patients who utilized nutrition counseling services. The analysis employed International Classification of Diseases, 10th edition, Clinical Modification (ICD-10-CM) diagnosis codes. We assessed the proportion of NAFLD patients who received nutrition counseling, comparing utilization across race, sex, US region, and income levels. Statistical analyses included chi-square tests for categorical variables and T-tests for continuous variables, conducted using SAS version 9.4
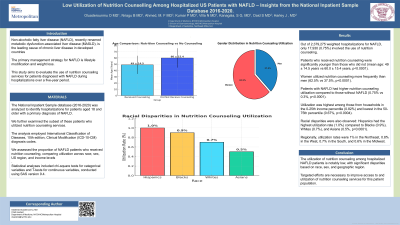
Results: Out of 2,379,275 weighted hospitalizations for NAFLD, only 17,930 (0.75%) involved the use of nutrition counseling. Patients who received nutrition counseling were significantly younger than those who did not (mean age: 49 ± 14.5 years vs 60.0 ± 15.4 years, p< 0.0001). Women utilized nutrition counseling more frequently than men (62.5% vs 37.5%, p< 0.0001). Patients with NAFLD had higher nutrition counseling utilization compared to those without NAFLD (0.75% vs 0.3%, p< 0.0001). Utilization was highest among those from households in the 0-25th income percentile (0.82%) and lowest in the 50-75th percentile (0.67%, p=0.0004). Racial disparities were also observed: Hispanics had the highest utilization rate (1.0%) compared to Blacks (0.9%), Whites (0.7%), and Asians (0.5%, p< 0.0001). Regionally, utilization rates were 1% in the Northeast, 0.8% in the West, 0.7% in the South, and 0.6% in the Midwest
Discussion: The utilization of nutrition counseling among hospitalized NAFLD patients is notably low, with significant disparities based on race, sex, and geographic region. Targeted efforts are necessary to improve access to and utilization of nutrition counseling services for this patient population
Disclosures:
Oladimeji E. Oluaderounmu, MD1, Bede N. Nriagu, MD, MPH1, Mirza Fawad Ahmed, MD1, Pushkar Kumar, MBBS, MD2, Nicole E. Villa, MD1, Sai Gautham Kanagala, MD1, Sarav Daid, MD2, Jennifer Harley, MD1. P1438 - Low Utilization of Nutrition Counselling Among Hospitalized US Patients with NAFLD – Insights from the National Inpatient Sample Database 2016-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Metropolitan, New York, NY; 2New York Medical College, New York, NY
Introduction: Non-alcoholic fatty liver disease (NAFLD), recently renamed metabolic dysfunction-associated liver disease (MASLD), is the leading cause of chronic liver disease in developed countries, with its prevalence and economic impact on the rise. The primary management strategy for NAFLD is lifestyle modification and weight loss. This study aims to evaluate the use of nutrition counseling services for patients diagnosed with NAFLD during hospitalizations over a five-year period
Methods: The National Inpatient Sample database (2016-2020) was analyzed to identify hospitalizations for patients aged 18 and older with a primary diagnosis of NAFLD. We further examined the subset of these patients who utilized nutrition counseling services. The analysis employed International Classification of Diseases, 10th edition, Clinical Modification (ICD-10-CM) diagnosis codes. We assessed the proportion of NAFLD patients who received nutrition counseling, comparing utilization across race, sex, US region, and income levels. Statistical analyses included chi-square tests for categorical variables and T-tests for continuous variables, conducted using SAS version 9.4
Results: Out of 2,379,275 weighted hospitalizations for NAFLD, only 17,930 (0.75%) involved the use of nutrition counseling. Patients who received nutrition counseling were significantly younger than those who did not (mean age: 49 ± 14.5 years vs 60.0 ± 15.4 years, p< 0.0001). Women utilized nutrition counseling more frequently than men (62.5% vs 37.5%, p< 0.0001). Patients with NAFLD had higher nutrition counseling utilization compared to those without NAFLD (0.75% vs 0.3%, p< 0.0001). Utilization was highest among those from households in the 0-25th income percentile (0.82%) and lowest in the 50-75th percentile (0.67%, p=0.0004). Racial disparities were also observed: Hispanics had the highest utilization rate (1.0%) compared to Blacks (0.9%), Whites (0.7%), and Asians (0.5%, p< 0.0001). Regionally, utilization rates were 1% in the Northeast, 0.8% in the West, 0.7% in the South, and 0.6% in the Midwest
Discussion: The utilization of nutrition counseling among hospitalized NAFLD patients is notably low, with significant disparities based on race, sex, and geographic region. Targeted efforts are necessary to improve access to and utilization of nutrition counseling services for this patient population
Disclosures:
Oladimeji Oluaderounmu indicated no relevant financial relationships.
Bede Nriagu indicated no relevant financial relationships.
Mirza Fawad Ahmed indicated no relevant financial relationships.
Pushkar Kumar indicated no relevant financial relationships.
Nicole Villa indicated no relevant financial relationships.
Sai Gautham Kanagala indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Oladimeji E. Oluaderounmu, MD1, Bede N. Nriagu, MD, MPH1, Mirza Fawad Ahmed, MD1, Pushkar Kumar, MBBS, MD2, Nicole E. Villa, MD1, Sai Gautham Kanagala, MD1, Sarav Daid, MD2, Jennifer Harley, MD1. P1438 - Low Utilization of Nutrition Counselling Among Hospitalized US Patients with NAFLD – Insights from the National Inpatient Sample Database 2016-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
