Sunday Poster Session
Category: Liver
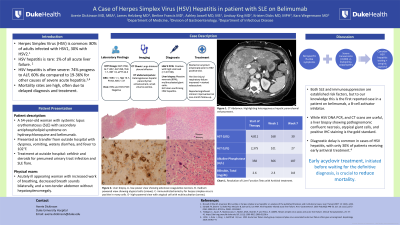
P1363 - A Case of Herpes Simplex Virus Hepatitis in Patient With SLE on Belimumab
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Averie Dickinson, MD, MBA
Duke University Health System
Durham, NC
Presenting Author(s)
Averie Dickinson, MD, MBA1, James Helzberg, MD1, Berline Francis, MD1, Ashley Jowell, MD2, Lindsay Y. King, MD1, Kristen Dicks, MD, MPH1, Kara Wegermann, MD1
1Duke University Health System, Durham, NC; 2Duke University Medical Center, Durham, NC
Introduction: Prompt clinical suspicion and early initiation of acyclovir for HSV hepatitis in patients presenting with nonspecific symptoms and acute liver injury are crucial to reducing mortality.
Case Description/Methods: A 54 year old woman with systemic lupus erythematosus (SLE) with secondary antiphospholipid syndrome on hydroxychloroquine and belimumab presented with dyspnea, vomiting, diarrhea, and fever to 102°F after recent treatment with cefdinir and steroids for presumed urinary tract infection and SLE flare.
On admission, she was hypoxic (94% on 60% FiO2) and afebrile. Exam showed an acutely ill appearing woman with increased work of breathing, decreased breath sounds, and a non-tender abdomen without hepatosplenomegaly. Labs indicated acute liver injury with aspartate aminotransferase (AST) 2768, alanine aminotransferase (ALT) 1457, Alkaline Phosphatase (ALP) 295, Total bilirubin (Tbili) 1.7, INR 1.9, and pancytopenia. Hepatitis B and C PCR was negative. She was started on empiric acyclovir for suspected HSV hepatitis.
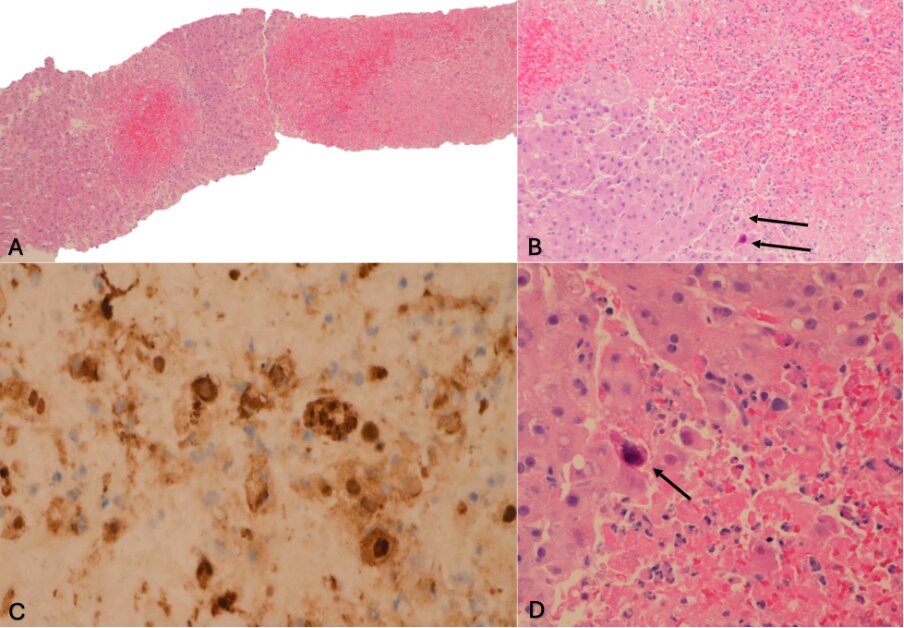
Over the next 24 hours, her liver tests worsened (AST 4811, ALT 2375, ALP 358, Tbili 3.2, INR 2.2), she developed progressive hypoxic respiratory failure, necessitating ICU transfer. Parainfluenza PCR returned positive. She was found to have positive serum HSV 2 PCR with high viral load ( >1.0 E+08). Liver biopsy showed massive necrosis (80%) and multinucleated giant cells, with IHC stain confirming HSV hepatitis diagnosis. Her liver injury and respiratory failure improved and she was transitioned to valacyclovir, for indefinite therapy. She reported significant improvement at her one-month follow-up hepatology visit.
Discussion: Although rare, HSV hepatitis carries a high mortality rate of up to 60%, compared to 19-36% for other causes of severe acute hepatitis. Clinical presentations are often non-specific, resembling flu-like symptoms such as fever, nausea, vomiting in immunocompromised or competent individuals. Both SLE and immunosuppression are established risk factors, but to our knowledge this is the first reported case in a patient on belimumab, a B-cell activator inhibitor. While HSV DNA PCR, and CT scans are useful, a liver biopsy showing pathognomonic confluent necrosis, atypical giant cells, and positive IHC staining is the gold standard. Diagnostic delay is common in cases of HSV hepatitis, with only 30% of patients receiving early antiviral treatment. Early acyclovir treatment, initiated before waiting for the definitive diagnosis, is crucial to reduce mortality.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Averie Dickinson, MD, MBA1, James Helzberg, MD1, Berline Francis, MD1, Ashley Jowell, MD2, Lindsay Y. King, MD1, Kristen Dicks, MD, MPH1, Kara Wegermann, MD1. P1363 - A Case of Herpes Simplex Virus Hepatitis in Patient With SLE on Belimumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Duke University Health System, Durham, NC; 2Duke University Medical Center, Durham, NC
Introduction: Prompt clinical suspicion and early initiation of acyclovir for HSV hepatitis in patients presenting with nonspecific symptoms and acute liver injury are crucial to reducing mortality.
Case Description/Methods: A 54 year old woman with systemic lupus erythematosus (SLE) with secondary antiphospholipid syndrome on hydroxychloroquine and belimumab presented with dyspnea, vomiting, diarrhea, and fever to 102°F after recent treatment with cefdinir and steroids for presumed urinary tract infection and SLE flare.
On admission, she was hypoxic (94% on 60% FiO2) and afebrile. Exam showed an acutely ill appearing woman with increased work of breathing, decreased breath sounds, and a non-tender abdomen without hepatosplenomegaly. Labs indicated acute liver injury with aspartate aminotransferase (AST) 2768, alanine aminotransferase (ALT) 1457, Alkaline Phosphatase (ALP) 295, Total bilirubin (Tbili) 1.7, INR 1.9, and pancytopenia. Hepatitis B and C PCR was negative. She was started on empiric acyclovir for suspected HSV hepatitis.
Over the next 24 hours, her liver tests worsened (AST 4811, ALT 2375, ALP 358, Tbili 3.2, INR 2.2), she developed progressive hypoxic respiratory failure, necessitating ICU transfer. Parainfluenza PCR returned positive. She was found to have positive serum HSV 2 PCR with high viral load ( >1.0 E+08). Liver biopsy showed massive necrosis (80%) and multinucleated giant cells, with IHC stain confirming HSV hepatitis diagnosis. Her liver injury and respiratory failure improved and she was transitioned to valacyclovir, for indefinite therapy. She reported significant improvement at her one-month follow-up hepatology visit.
Discussion: Although rare, HSV hepatitis carries a high mortality rate of up to 60%, compared to 19-36% for other causes of severe acute hepatitis. Clinical presentations are often non-specific, resembling flu-like symptoms such as fever, nausea, vomiting in immunocompromised or competent individuals. Both SLE and immunosuppression are established risk factors, but to our knowledge this is the first reported case in a patient on belimumab, a B-cell activator inhibitor. While HSV DNA PCR, and CT scans are useful, a liver biopsy showing pathognomonic confluent necrosis, atypical giant cells, and positive IHC staining is the gold standard. Diagnostic delay is common in cases of HSV hepatitis, with only 30% of patients receiving early antiviral treatment. Early acyclovir treatment, initiated before waiting for the definitive diagnosis, is crucial to reduce mortality.
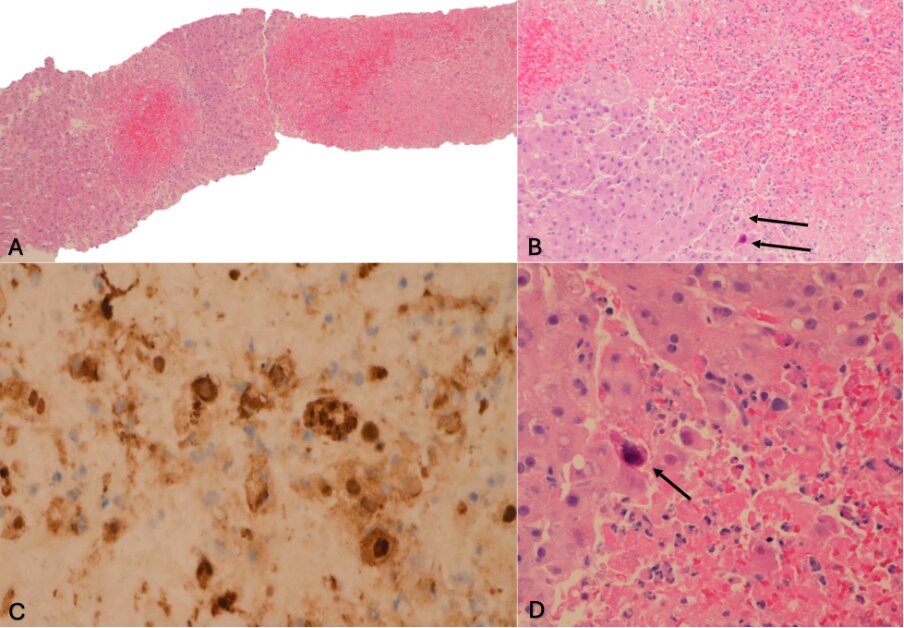
Figure: Figure 1. Liver biopsy. A- low-power view showing extensive coagulative necrosis. B- medium-powered view showing atypical cells (arrows). C- immunohistochemistry for herpes simplex virus is positive in many cells. D- high-powered view with atypical cell with multinucleation (arrow).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Averie Dickinson indicated no relevant financial relationships.
James Helzberg indicated no relevant financial relationships.
Berline Francis indicated no relevant financial relationships.
Ashley Jowell indicated no relevant financial relationships.
Lindsay King indicated no relevant financial relationships.
Kristen Dicks indicated no relevant financial relationships.
Kara Wegermann: Madrigal Pharmaceuticals – Study investigator. Mirum Pharmaceuticals – Study investigator.
Averie Dickinson, MD, MBA1, James Helzberg, MD1, Berline Francis, MD1, Ashley Jowell, MD2, Lindsay Y. King, MD1, Kristen Dicks, MD, MPH1, Kara Wegermann, MD1. P1363 - A Case of Herpes Simplex Virus Hepatitis in Patient With SLE on Belimumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
