Sunday Poster Session
Category: Liver
P1365 - Risankizumab-Associated Idiosyncratic Drug-Induced Liver Injury
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Vivek V. Jasti, MD
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Vivek V. Jasti, MD1, Anthony Michaels, MD2, Shail Govani, MD, MSc2
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Columbus, OH
Introduction: Idiosyncratic drug-induced liver injury (DILI) is a diagnostic challenge. Numerous culprit medications have been identified and presentation is variable. Risankizumab is a humanized monoclonal antibody to IL-23 that is FDA approved for the treatment of plaque psoriasis, psoriatic arthritis, and moderate-severe Crohn’s disease. We present a case of DILI most likely secondary to Risankizumab.
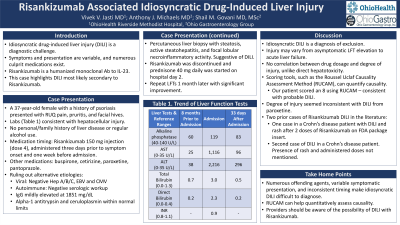
Case Description/Methods: A 37-year-old female with psoriasis presented with right upper quadrant pain, pruritis, and facial hives. Blood work revealed AST 1116, ALT 2216 U/L, and total bilirubin 3.0 mg/dL (direct bilirubin of 2.3 mg/dL). ALP and INR were normal. LFTs 8 months ago were unremarkable. She has no personal or family history of liver disease and no regular alcohol use. Her fourth injection of Risankizumab, 150 mg was 3 days prior to symptom onset and 1 week before admission. She also started paroxetine 4 months prior to admission. Hepatitis A, B, C, CMV and EBV were ruled out. Serologic workup for autoimmune hepatitis was negative. Serum IgG was mildly elevated at 1851 mg/dL. Alpha-1 antitrypsin and ceruloplasmin were normal. Percutaneous liver biopsy showed steatosis, active steatohepatitis, and focal lobular necroinflammatory activity, findings suggestive of DILI. Risankizumab was discontinued and prednisone 40 mg daily was started on hospital day 2. Repeat LFTs, 1 month later, revealed AST 96 U/L, ALT 296 U/L, and normal bilirubin.
Discussion: Idiosyncratic DILI is a clinical diagnosis of exclusion. Many offending agents including prescriptions, illicit drugs, and supplements have been identified. Liver injury can vary from asymptomatic to acute liver failure. Injury is not correlated to dosage, unlike drugs with direct hepatotoxicity. Currently, no specific biomarkers exist to distinguish DILI from other causes of liver injury. Scoring tools, such as the Roussel Uclaf Causality Assessment Method (RUCAM), can help quantitively assess causality. Using RUCAM our patient scored 8, consistent with probable DILI. The degree of injury seemed inconsistent with DILI from paroxetine.
Literature search revealed two prior instances of DILI with Risankizumab. The medication’s FDA package insert mentions one patient with Crohn’s disease who developed DILI and rash after 2 doses of Risankizumab. The second occurrence was in a young female with Crohn’s disease; no rash was mentioned. Mild LFT elevation has been reported with Risankizumab, but providers should be aware of the possibility of idiosyncratic DILI.
Disclosures:
Vivek V. Jasti, MD1, Anthony Michaels, MD2, Shail Govani, MD, MSc2. P1365 - Risankizumab-Associated Idiosyncratic Drug-Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Columbus, OH
Introduction: Idiosyncratic drug-induced liver injury (DILI) is a diagnostic challenge. Numerous culprit medications have been identified and presentation is variable. Risankizumab is a humanized monoclonal antibody to IL-23 that is FDA approved for the treatment of plaque psoriasis, psoriatic arthritis, and moderate-severe Crohn’s disease. We present a case of DILI most likely secondary to Risankizumab.
Case Description/Methods: A 37-year-old female with psoriasis presented with right upper quadrant pain, pruritis, and facial hives. Blood work revealed AST 1116, ALT 2216 U/L, and total bilirubin 3.0 mg/dL (direct bilirubin of 2.3 mg/dL). ALP and INR were normal. LFTs 8 months ago were unremarkable. She has no personal or family history of liver disease and no regular alcohol use. Her fourth injection of Risankizumab, 150 mg was 3 days prior to symptom onset and 1 week before admission. She also started paroxetine 4 months prior to admission. Hepatitis A, B, C, CMV and EBV were ruled out. Serologic workup for autoimmune hepatitis was negative. Serum IgG was mildly elevated at 1851 mg/dL. Alpha-1 antitrypsin and ceruloplasmin were normal. Percutaneous liver biopsy showed steatosis, active steatohepatitis, and focal lobular necroinflammatory activity, findings suggestive of DILI. Risankizumab was discontinued and prednisone 40 mg daily was started on hospital day 2. Repeat LFTs, 1 month later, revealed AST 96 U/L, ALT 296 U/L, and normal bilirubin.
Discussion: Idiosyncratic DILI is a clinical diagnosis of exclusion. Many offending agents including prescriptions, illicit drugs, and supplements have been identified. Liver injury can vary from asymptomatic to acute liver failure. Injury is not correlated to dosage, unlike drugs with direct hepatotoxicity. Currently, no specific biomarkers exist to distinguish DILI from other causes of liver injury. Scoring tools, such as the Roussel Uclaf Causality Assessment Method (RUCAM), can help quantitively assess causality. Using RUCAM our patient scored 8, consistent with probable DILI. The degree of injury seemed inconsistent with DILI from paroxetine.
Literature search revealed two prior instances of DILI with Risankizumab. The medication’s FDA package insert mentions one patient with Crohn’s disease who developed DILI and rash after 2 doses of Risankizumab. The second occurrence was in a young female with Crohn’s disease; no rash was mentioned. Mild LFT elevation has been reported with Risankizumab, but providers should be aware of the possibility of idiosyncratic DILI.
Disclosures:
Vivek Jasti indicated no relevant financial relationships.
Anthony Michaels: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Madrigal – Speakers Bureau.
Shail Govani: Abbvie – Speakers Bureau. Bristol Meyers Squibb – Speakers Bureau.
Vivek V. Jasti, MD1, Anthony Michaels, MD2, Shail Govani, MD, MSc2. P1365 - Risankizumab-Associated Idiosyncratic Drug-Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
