Sunday Poster Session
Category: Liver
P1367 - Budd-Chiari Plus a Friend - A Case of Chronic Budd Chiari Syndrome and Simultaneous Superior Mesenteric Vein Thrombus
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Anastasia Naritsin, DO
Lahey Hospital and Medical Center
Burlington, MA
Presenting Author(s)
Anastasia Naritsin, DO, Maisa Elbadawi, MD, Atoussa Goldar-Najafi, MD, Raza Malik, MD
Lahey Hospital and Medical Center, Burlington, MA
Introduction: Budd-Chiari Syndrome (BCS) is an obstruction of the hepatic venous outflow tract occurring in 1 in 100,000 people worldwide. Obstruction can occur from the small hepatic veins to the junction of the inferior vena cava and right atrium. Common etiologies include inherited thrombophilias and myeloproliferative neoplasms. BCS is difficult to diagnose and is based on clinical and laboratory findings with radiologic evidence of large vessel venous drainage impairment or histological evidence of small vessel obstruction.
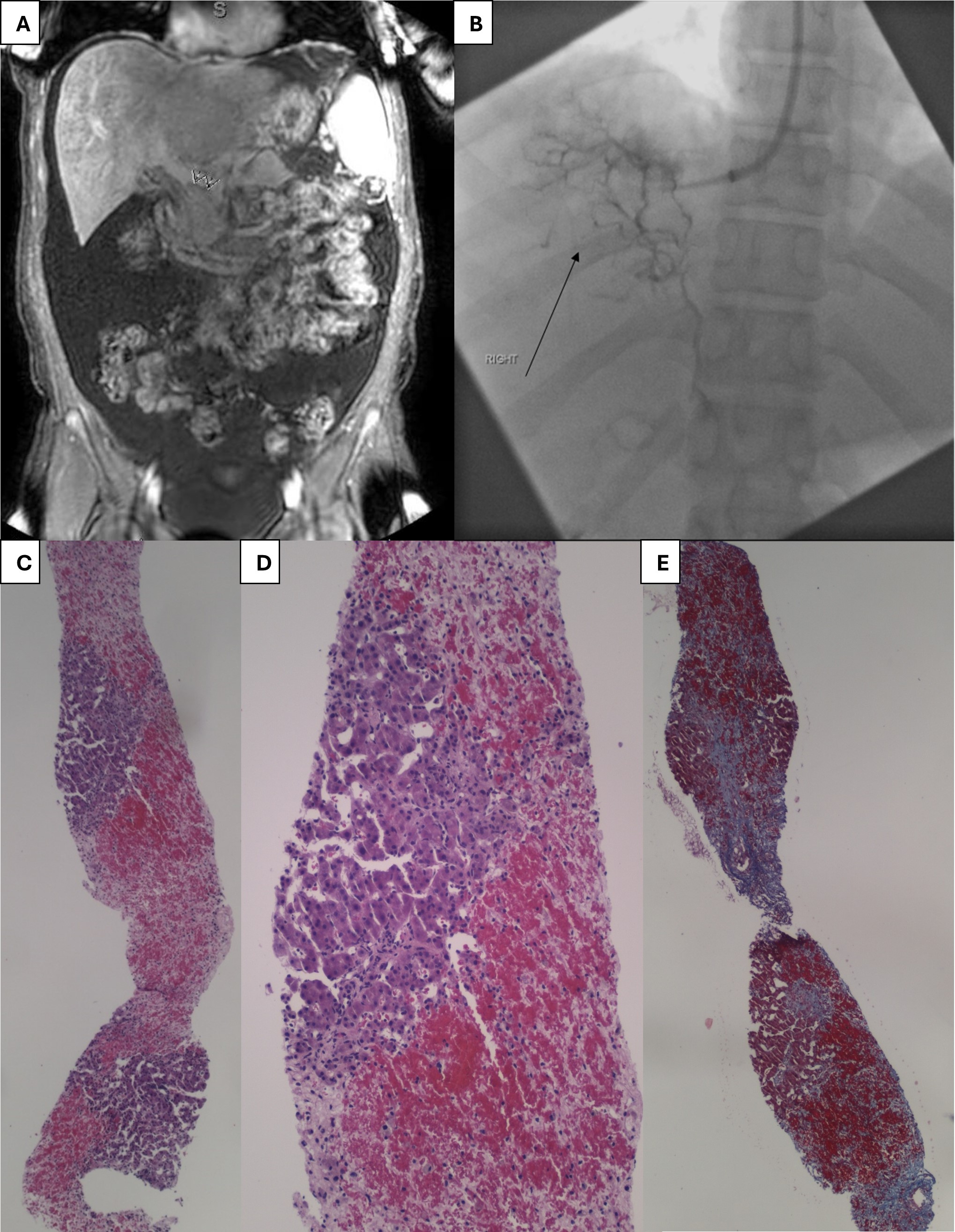
Case Description/Methods: 24-year-old patient with factor V Leiden mutation and PCOS presents with abdominal distension and jaundice. Patient was hemodynamically stable and labs showed AST 102, ALT 149, total bilirubin 8, INR 1.71, and normal CBC. Abdominal ultrasound showed large volume ascites, patent major hepatic vessels, and hepatic vein thinning. CT abdomen showed inhomogeneous hepatic parenchymal density with splenomegaly, extensive upper abdominal venous collaterals, and poorly visualized hepatic vessels. MRCP showed cirrhotic morphology, portal venous hypertension, SMV thrombus extending to the main portal vein, and no biliary obstruction (Figure 1). Peritoneal fluid had SAAG 2.5 and total protein < 2. Viral, toxin, and liver serologies were unremarkable. Patient was taking a Chinese herbal supplement, so DILI was suspected and managed per NAC protocol. A hepatic venogram revealed no patent hepatic veins consistent with chronic occlusion and on puncturing into the liver parenchyma with innumerable collateral veins in a “spider web” pattern. Liver biopsy showed pericentral hepatocytic loss, parenchymal necrosis and congestion, acute on chronic portal inflammation, pericentral parenchymal collapse, bridging necrosis and foci of portal bridging fibrosis consistent with BCS (Figure 1). Pt was evaluated for direct intrahepatic portocaval shunt (DIPS) but with anticoagulation and diuretics, patient's thrombus, ascites and MELD-Na improved.
Discussion: As in this case, imaging isn't always reliable, especially with small vessel involvement, so liver biopsy is integral, even if alternative pathology is suspected. Management of this case was challenging as the patient presented with chronic BCS complicated by cirrhosis and simultaneous SMV thrombus. Given patients’ marked improvement with systemic anticoagulation and underlying cirrhosis, there was a multidisciplinary decision to evaluate and list for liver transplant and avoid DIPS due to the risk of liver decompensation and failure.
Disclosures:
Anastasia Naritsin, DO, Maisa Elbadawi, MD, Atoussa Goldar-Najafi, MD, Raza Malik, MD. P1367 - Budd-Chiari Plus a Friend - A Case of Chronic Budd Chiari Syndrome and Simultaneous Superior Mesenteric Vein Thrombus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lahey Hospital and Medical Center, Burlington, MA
Introduction: Budd-Chiari Syndrome (BCS) is an obstruction of the hepatic venous outflow tract occurring in 1 in 100,000 people worldwide. Obstruction can occur from the small hepatic veins to the junction of the inferior vena cava and right atrium. Common etiologies include inherited thrombophilias and myeloproliferative neoplasms. BCS is difficult to diagnose and is based on clinical and laboratory findings with radiologic evidence of large vessel venous drainage impairment or histological evidence of small vessel obstruction.
Case Description/Methods: 24-year-old patient with factor V Leiden mutation and PCOS presents with abdominal distension and jaundice. Patient was hemodynamically stable and labs showed AST 102, ALT 149, total bilirubin 8, INR 1.71, and normal CBC. Abdominal ultrasound showed large volume ascites, patent major hepatic vessels, and hepatic vein thinning. CT abdomen showed inhomogeneous hepatic parenchymal density with splenomegaly, extensive upper abdominal venous collaterals, and poorly visualized hepatic vessels. MRCP showed cirrhotic morphology, portal venous hypertension, SMV thrombus extending to the main portal vein, and no biliary obstruction (Figure 1). Peritoneal fluid had SAAG 2.5 and total protein < 2. Viral, toxin, and liver serologies were unremarkable. Patient was taking a Chinese herbal supplement, so DILI was suspected and managed per NAC protocol. A hepatic venogram revealed no patent hepatic veins consistent with chronic occlusion and on puncturing into the liver parenchyma with innumerable collateral veins in a “spider web” pattern. Liver biopsy showed pericentral hepatocytic loss, parenchymal necrosis and congestion, acute on chronic portal inflammation, pericentral parenchymal collapse, bridging necrosis and foci of portal bridging fibrosis consistent with BCS (Figure 1). Pt was evaluated for direct intrahepatic portocaval shunt (DIPS) but with anticoagulation and diuretics, patient's thrombus, ascites and MELD-Na improved.
Discussion: As in this case, imaging isn't always reliable, especially with small vessel involvement, so liver biopsy is integral, even if alternative pathology is suspected. Management of this case was challenging as the patient presented with chronic BCS complicated by cirrhosis and simultaneous SMV thrombus. Given patients’ marked improvement with systemic anticoagulation and underlying cirrhosis, there was a multidisciplinary decision to evaluate and list for liver transplant and avoid DIPS due to the risk of liver decompensation and failure.
Figure: A. Superior Mesenteric Vein and Portal Vein Thrombus
B. Hepatic Venogram
C. Low power view showing pericentral parenchymal congestion and hepatocytic loss
D. Parenchymal hemorrhagic necrosis
E. Trichrome stain showing bridging fibrosis and focal nodule formation
B. Hepatic Venogram
C. Low power view showing pericentral parenchymal congestion and hepatocytic loss
D. Parenchymal hemorrhagic necrosis
E. Trichrome stain showing bridging fibrosis and focal nodule formation
Disclosures:
Anastasia Naritsin indicated no relevant financial relationships.
Maisa Elbadawi indicated no relevant financial relationships.
Atoussa Goldar-Najafi indicated no relevant financial relationships.
Raza Malik indicated no relevant financial relationships.
Anastasia Naritsin, DO, Maisa Elbadawi, MD, Atoussa Goldar-Najafi, MD, Raza Malik, MD. P1367 - Budd-Chiari Plus a Friend - A Case of Chronic Budd Chiari Syndrome and Simultaneous Superior Mesenteric Vein Thrombus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
