Sunday Poster Session
Category: Liver
P1368 - Rare Case of Splenic Artery Steal Syndrome Resulting in Persistent Ascites in a Patient Post-Liver Transplant
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Has Audio
- TL
Tayna Latortue, MD
University of Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Tayna Latortue, MD1, Devika Dixit, MD1, Calvin Kiani, MD1, Andreas Zori, MD1, Nimy John, MD2
1University of Florida College of Medicine, Gainesville, FL; 2University of Florida College of Medicine, Newberry, FL
Introduction: Post liver transplant ascites is seen in 5 -7% of patients post transplant. Common causes include impaired graft outflow, recurrent HCV infection, and peritonitis. In 30% of cases, etiology is unknown. Ascites resolves in 6 months in 75% of cases.
Splenic Artery Steal Syndrome (SASS) is a rare complication of liver transplant. SASS can cause ascites due to increased portal profusions as a result of a competitive shunt of blood to the splenic artery away from the celiac trunk and hepatic artery. It leads to graft ischemia after liver transplant and cause biliary ischemia, ascites, and, rarely, graft failure. We present a case of SASS leading to diuretic refractory ascites in a post liver transplant patient.
Case Description/Methods: A 45-year-old male with a PMH of Non-alcoholic steatohepatitis cirrhosis received an orthotopic liver transplant with end-to-end choledo-choledochostomy biliary anastomoses. Post-liver transplant, patient continued to have large ascites. Ascites did not respond to high-dose diuretics and required repeated paracentesis. Patient underwent extensive workup to rule out hepatic artery stenosis, HCV infection, IVC obstruction,Peritonitis and cardiac failure. He had a transjugular liver biopsy showing no signs of rejection, inflammatory infiltrates or fibrosis and a hepatic vein pressure gradient of 5. CT scan of the liver showed a patent hepatic artery, patent portal vein, splenomegaly, and several portosystemic collaterals.
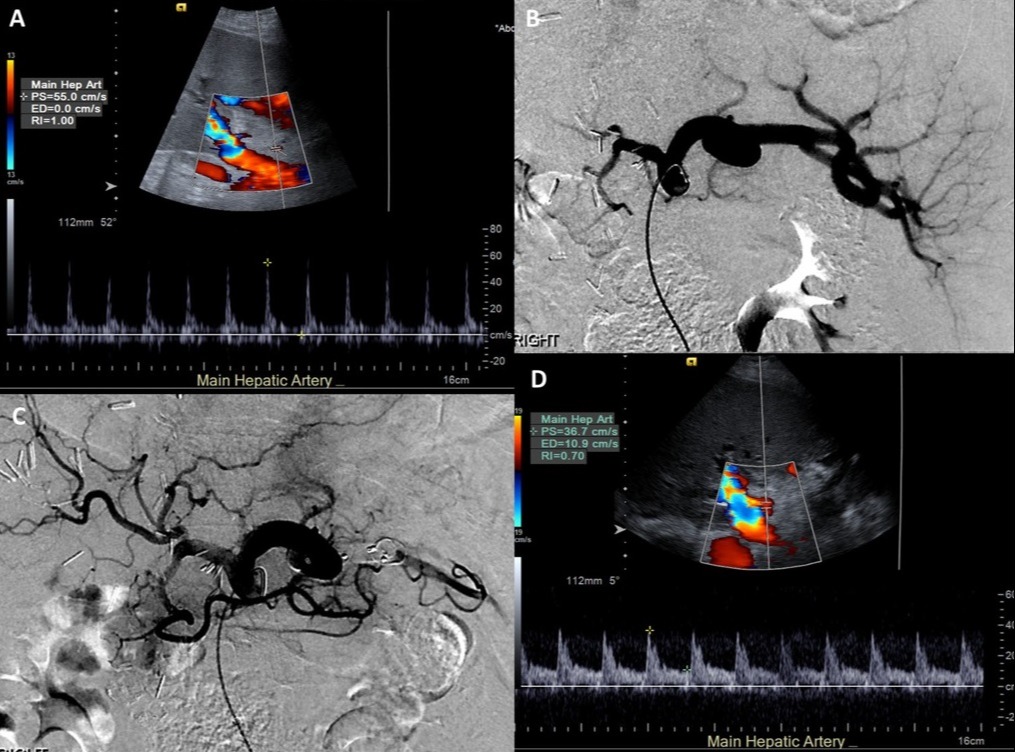
Ultrasound of abdomen was concerning for high resistive index in the hepatic artery. CT angiography of celiac artery showed a large tortuous splenic artery with significantly diminished flow in the hepatic artery. This was concerning for SASS. He was referred to IR and he underwent proximal splenic artery embolization. Post-embolization angiograms showed increased flow within hepatic arteries. Splenic perfusion was maintained via collaterals. Post embolization, he was followed in clinic and his ascites resolved.
Discussion: Incidence of SASS in post-liver transplant patients is estimated between 0.6% and 10%. There are no definitive ultrasound findings, however high resistive index (RI > 0.8) and hepatic artery velocity above 100 cm/s in the absence of hepatic artery stenosis is commonly observed. Celiac artery angiography is the most specific finding in SASS and demonstrates preferential flow to the splenic artery associated with either a large splenic artery or multiple collaterals. Splenic artery or collateral embolization is the treatment of choice.
Disclosures:
Tayna Latortue, MD1, Devika Dixit, MD1, Calvin Kiani, MD1, Andreas Zori, MD1, Nimy John, MD2. P1368 - Rare Case of Splenic Artery Steal Syndrome Resulting in Persistent Ascites in a Patient Post-Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Gainesville, FL; 2University of Florida College of Medicine, Newberry, FL
Introduction: Post liver transplant ascites is seen in 5 -7% of patients post transplant. Common causes include impaired graft outflow, recurrent HCV infection, and peritonitis. In 30% of cases, etiology is unknown. Ascites resolves in 6 months in 75% of cases.
Splenic Artery Steal Syndrome (SASS) is a rare complication of liver transplant. SASS can cause ascites due to increased portal profusions as a result of a competitive shunt of blood to the splenic artery away from the celiac trunk and hepatic artery. It leads to graft ischemia after liver transplant and cause biliary ischemia, ascites, and, rarely, graft failure. We present a case of SASS leading to diuretic refractory ascites in a post liver transplant patient.
Case Description/Methods: A 45-year-old male with a PMH of Non-alcoholic steatohepatitis cirrhosis received an orthotopic liver transplant with end-to-end choledo-choledochostomy biliary anastomoses. Post-liver transplant, patient continued to have large ascites. Ascites did not respond to high-dose diuretics and required repeated paracentesis. Patient underwent extensive workup to rule out hepatic artery stenosis, HCV infection, IVC obstruction,Peritonitis and cardiac failure. He had a transjugular liver biopsy showing no signs of rejection, inflammatory infiltrates or fibrosis and a hepatic vein pressure gradient of 5. CT scan of the liver showed a patent hepatic artery, patent portal vein, splenomegaly, and several portosystemic collaterals.
Ultrasound of abdomen was concerning for high resistive index in the hepatic artery. CT angiography of celiac artery showed a large tortuous splenic artery with significantly diminished flow in the hepatic artery. This was concerning for SASS. He was referred to IR and he underwent proximal splenic artery embolization. Post-embolization angiograms showed increased flow within hepatic arteries. Splenic perfusion was maintained via collaterals. Post embolization, he was followed in clinic and his ascites resolved.
Discussion: Incidence of SASS in post-liver transplant patients is estimated between 0.6% and 10%. There are no definitive ultrasound findings, however high resistive index (RI > 0.8) and hepatic artery velocity above 100 cm/s in the absence of hepatic artery stenosis is commonly observed. Celiac artery angiography is the most specific finding in SASS and demonstrates preferential flow to the splenic artery associated with either a large splenic artery or multiple collaterals. Splenic artery or collateral embolization is the treatment of choice.
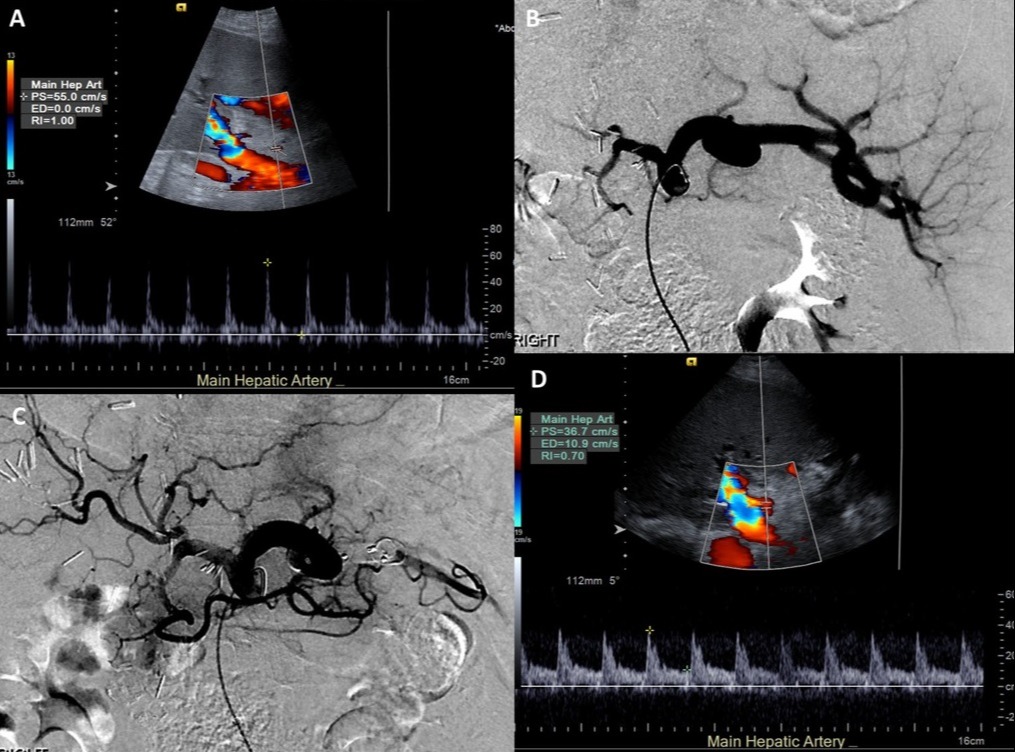
Figure: Figure - SASS before (A-B) and after SAE (C-D)
Disclosures:
Tayna Latortue indicated no relevant financial relationships.
Devika Dixit indicated no relevant financial relationships.
Calvin Kiani indicated no relevant financial relationships.
Andreas Zori indicated no relevant financial relationships.
Nimy John indicated no relevant financial relationships.
Tayna Latortue, MD1, Devika Dixit, MD1, Calvin Kiani, MD1, Andreas Zori, MD1, Nimy John, MD2. P1368 - Rare Case of Splenic Artery Steal Syndrome Resulting in Persistent Ascites in a Patient Post-Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
