Sunday Poster Session
Category: Liver
P1370 - Diagnosing Hepatic Sarcoidosis: An Uncommon Presentation of Sarcoidosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AC
Ashleigh Chuah, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Ashleigh Chuah, MD, Cynthia Tran, MD, Saurabh Chawla, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Biliary strictures can arise from malignant, infectious, autoimmune, or inflammatory conditions. Hepatic sarcoidosis (HS) is a rare cause. Diagnosing HS is crucial for timely and effective treatment.
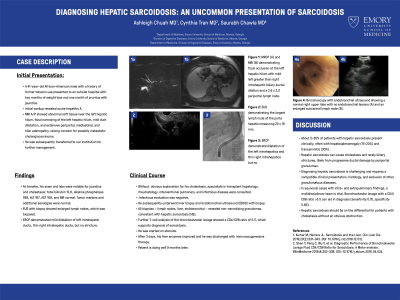
Case Description/Methods: A 41-year-old African-American male with a history of former tobacco use presented to an outside hospital with two months of weight loss and one month of pruritus with jaundice. Initial workup revealed acute hepatitis A. Magnetic resonance imaging showed abnormal soft tissue near the left hepatic hilum, focal narrowing of the left hepatic hilum, mild duct dilatation, and extensive periportal, mediastinal, and hilar adenopathy. Findings were concerning for possible metastatic cholangiocarcinoma. He was subsequently transferred to our institution.
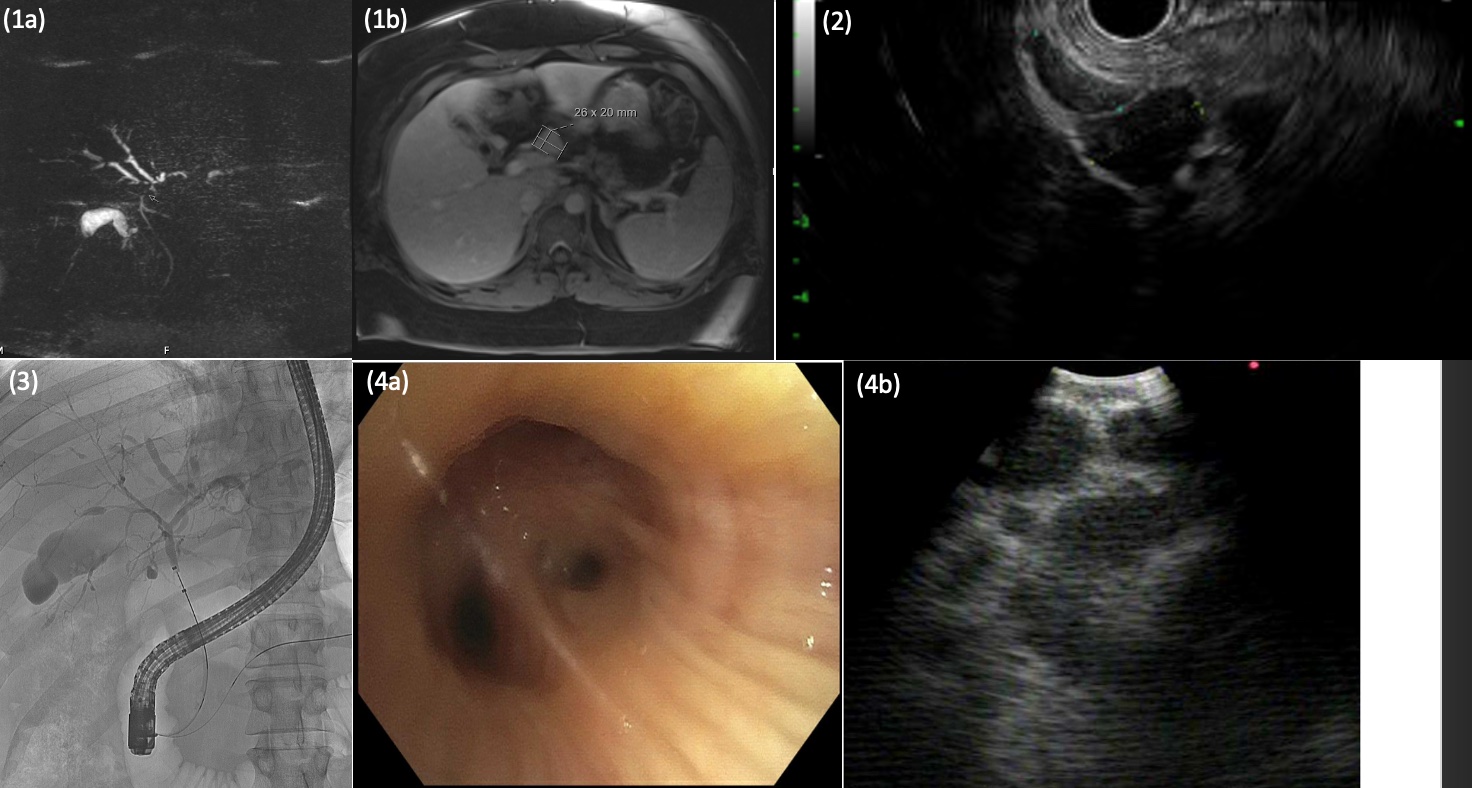
At transfer, his exam and labs were notable for jaundice and cholestasis: total bilirubin 12.6, alkaline phosphatase 959, alanine aminotransferase 167, aspartate aminotransferase 108, and international normalization ratio normal. Tumor markers and additional serologies were normal. An endoscopic ultrasound (EUS) with biopsy showed enlarged lymph nodes. Subsequent endoscopic retrograde cholangiopancreatography (ERCP) demonstrated mild dilatation of the left intrahepatics and thin right intrahepatics but no stricture. Without an obvious explanation for his cholestasis, specialists in transplant hepatology, rheumatology, interventional pulmonary, and infectious disease were consulted. The infectious disease evaluation was negative. He underwent liver biopsy and endobronchial ultrasound (EBUS) with biopsy. All biopsies – lymph nodes, liver, endobronchial – revealed non-necrotizing granulomas. Further T-cell analysis of the bronchoalveolar lavage showed a CD4/CD8 ratio of 5.5, suggestive of sarcoidosis. He was started on high-dose steroids. After 3 days, his liver enzymes improved and he was discharged with immunosuppressive therapy. He is doing well 9 months later.
Discussion: Only a minority of patients (5-30%) with HS present clinically, often with hepatosplenomegaly (15-20%) and transaminitis (30%) and only rarely with biliary strictures. Diagnosing HS is challenging and requires a compatible clinical presentation, histology, and exclusion of other granulomatous diseases. In equivocal cases with intra- and extrapulmonary findings, a multidisciplinary team is vital. Bronchoalveolar lavage with a CD4/CD8 ratio >3.5 can aid in diagnosis (sensitivity 0.70, specificity 0.83).
Disclosures:
Ashleigh Chuah, MD, Cynthia Tran, MD, Saurabh Chawla, MD. P1370 - Diagnosing Hepatic Sarcoidosis: An Uncommon Presentation of Sarcoidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Biliary strictures can arise from malignant, infectious, autoimmune, or inflammatory conditions. Hepatic sarcoidosis (HS) is a rare cause. Diagnosing HS is crucial for timely and effective treatment.
Case Description/Methods: A 41-year-old African-American male with a history of former tobacco use presented to an outside hospital with two months of weight loss and one month of pruritus with jaundice. Initial workup revealed acute hepatitis A. Magnetic resonance imaging showed abnormal soft tissue near the left hepatic hilum, focal narrowing of the left hepatic hilum, mild duct dilatation, and extensive periportal, mediastinal, and hilar adenopathy. Findings were concerning for possible metastatic cholangiocarcinoma. He was subsequently transferred to our institution.
At transfer, his exam and labs were notable for jaundice and cholestasis: total bilirubin 12.6, alkaline phosphatase 959, alanine aminotransferase 167, aspartate aminotransferase 108, and international normalization ratio normal. Tumor markers and additional serologies were normal. An endoscopic ultrasound (EUS) with biopsy showed enlarged lymph nodes. Subsequent endoscopic retrograde cholangiopancreatography (ERCP) demonstrated mild dilatation of the left intrahepatics and thin right intrahepatics but no stricture. Without an obvious explanation for his cholestasis, specialists in transplant hepatology, rheumatology, interventional pulmonary, and infectious disease were consulted. The infectious disease evaluation was negative. He underwent liver biopsy and endobronchial ultrasound (EBUS) with biopsy. All biopsies – lymph nodes, liver, endobronchial – revealed non-necrotizing granulomas. Further T-cell analysis of the bronchoalveolar lavage showed a CD4/CD8 ratio of 5.5, suggestive of sarcoidosis. He was started on high-dose steroids. After 3 days, his liver enzymes improved and he was discharged with immunosuppressive therapy. He is doing well 9 months later.
Discussion: Only a minority of patients (5-30%) with HS present clinically, often with hepatosplenomegaly (15-20%) and transaminitis (30%) and only rarely with biliary strictures. Diagnosing HS is challenging and requires a compatible clinical presentation, histology, and exclusion of other granulomatous diseases. In equivocal cases with intra- and extrapulmonary findings, a multidisciplinary team is vital. Bronchoalveolar lavage with a CD4/CD8 ratio >3.5 can aid in diagnosis (sensitivity 0.70, specificity 0.83).
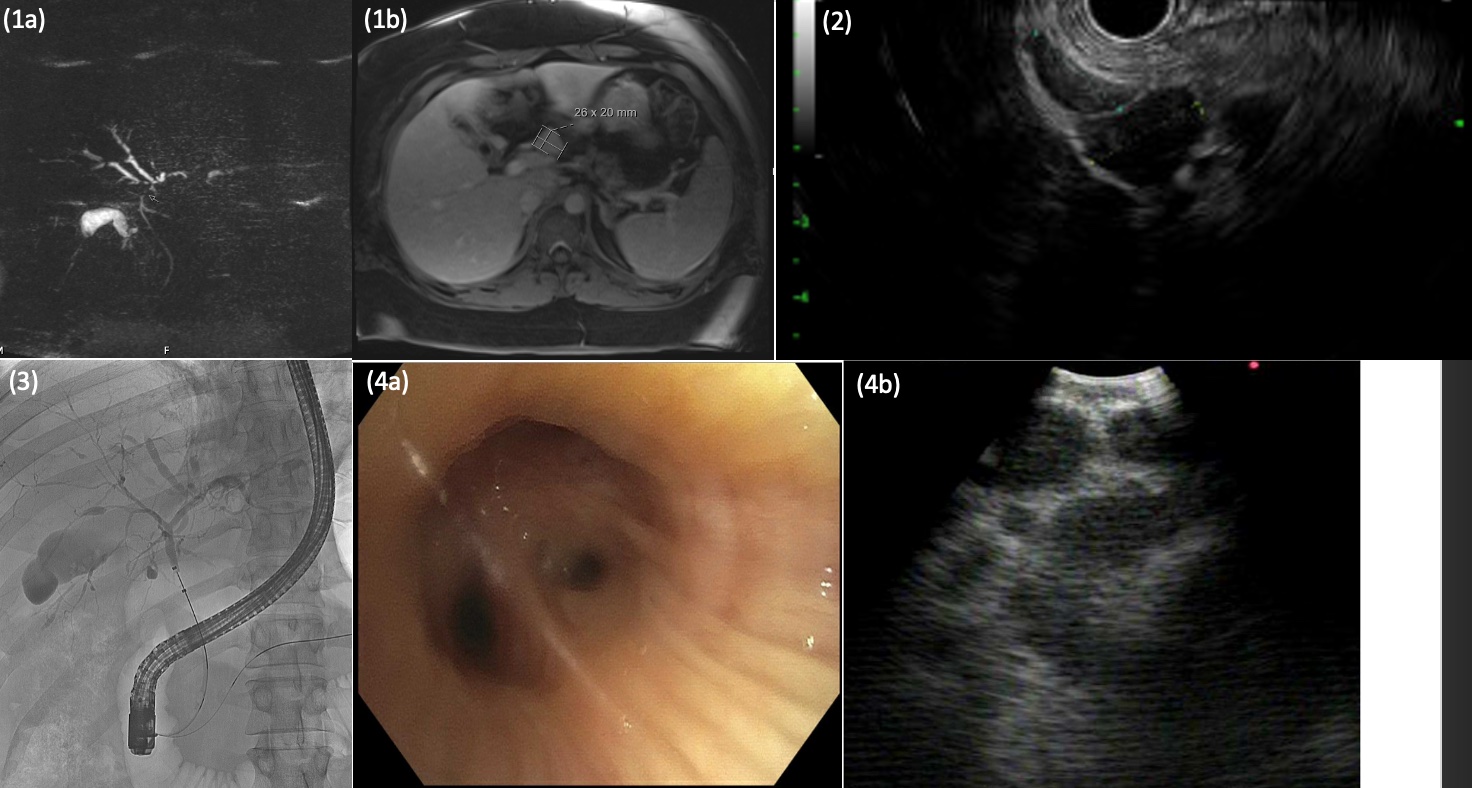
Figure: Figure 1A and 1B: Magnetic resonance cholangiopancreatography (A) and magnetic resonance imaging (B) showing focal occlusion at the left hepatic hilum with mild left greater than right intrahepatic biliary ductal dilation and a 2.6 x 2.0 periportal lymph node.
Figure 2: Endoscopic ultrasound showing the largest lymph node at the porta hepatis measuring 23 x 16 mm.
Figure 3: Endoscopic retrograde cholangiopancreatography showing dilatation of the left intrahepatics and thin right intrahepatics but no stricture.
Figure 4: Bronchoscopy with endobronchial ultrasound showing a normal right upper lobe with no endobronchial lesions (A) and an enlarged subcarinal lymph node (B).
Figure 2: Endoscopic ultrasound showing the largest lymph node at the porta hepatis measuring 23 x 16 mm.
Figure 3: Endoscopic retrograde cholangiopancreatography showing dilatation of the left intrahepatics and thin right intrahepatics but no stricture.
Figure 4: Bronchoscopy with endobronchial ultrasound showing a normal right upper lobe with no endobronchial lesions (A) and an enlarged subcarinal lymph node (B).
Disclosures:
Ashleigh Chuah indicated no relevant financial relationships.
Cynthia Tran indicated no relevant financial relationships.
Saurabh Chawla indicated no relevant financial relationships.
Ashleigh Chuah, MD, Cynthia Tran, MD, Saurabh Chawla, MD. P1370 - Diagnosing Hepatic Sarcoidosis: An Uncommon Presentation of Sarcoidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
