Sunday Poster Session
Category: Liver
P1279 - A Curious Case of Chylous Ascites
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kadon Caskey, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Kadon Caskey, MD1, Marina Ngassa, MD1, Sarika Ziemann, MD2
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Chylous ascites is lymphatic fluid within the peritoneal cavity and is an uncommon condition. Its occurrence in esophageal cancer is rare and presents diagnostic and therapeutic challenges. Through this case, we aim to review the evaluation, diagnosis, and management of chylous ascites.
Case Description/Methods: The patient is a 52-year-old male with poorly differentiated esophageal carcinoma diagnosed by lymph node biopsy and currently receiving chemotherapy and immunotherapy who is admitted for worsening anasarca refractory to diuretics. Two months ago, he developed volume overload and exertional dyspnea after receiving nivolumab. At the time, he was presumed to have immune checkpoint inhibitor myocarditis due to his elevated cardiac troponin and coronary angiogram with non-obstructive disease, and he was empirically treated with systemic steroids. He also received oral diuretics for presumed new-onset heart failure with preserved ejection fraction.
During this admission, a paracentesis revealed chylous ascites with triglycerides >5000 mg/dL and thoracentesis showed chylothorax. Cytology was negative for malignancy. A computed tomographic (CT) scan showed a 3.2 cm x 2.7 cm paraesophageal lymphocele. Despite treatment with diuretics, a low-fat diet, and paracentesis, his chylous fluid reaccumulated. A multidisciplinary team attempted thoracic duct embolization but were unsuccessful. The patient continues to receive serial therapeutic paracenteses and thoracenteses.
Discussion: Clinicians should maintain a broad differential when evaluating patients with new ascites. Guidelines recommend diagnostic paracentesis in all patients with clinically evident new ascites. Chylous ascites is defined by triglyceride levels >200 mg/dL. It most commonly occurs in lymphatic anomalies or malignancy but can also be caused by cirrhosis, infection, and other less common etiologies. CT scans are helpful to determine the underlying etiology in patients with malignancy or recent surgeries. Lymphoscintigraphy and lymphangiography can assess for lymphatic obstruction or leakage and are considered the gold standard. Treatment is multifarious and relies on dietary adjustments, pharmacologic therapies, and more invasive interventions depending on the etiology. We hypothesize our patient’s lymph node biopsy led to lymphocele formation and resulting lymphatic obstruction. This case emphasizes the importance of paracentesis in evaluating new ascites and the often challenging nature of managing chylous fluid collections.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kadon Caskey, MD1, Marina Ngassa, MD1, Sarika Ziemann, MD2. P1279 - A Curious Case of Chylous Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Chylous ascites is lymphatic fluid within the peritoneal cavity and is an uncommon condition. Its occurrence in esophageal cancer is rare and presents diagnostic and therapeutic challenges. Through this case, we aim to review the evaluation, diagnosis, and management of chylous ascites.
Case Description/Methods: The patient is a 52-year-old male with poorly differentiated esophageal carcinoma diagnosed by lymph node biopsy and currently receiving chemotherapy and immunotherapy who is admitted for worsening anasarca refractory to diuretics. Two months ago, he developed volume overload and exertional dyspnea after receiving nivolumab. At the time, he was presumed to have immune checkpoint inhibitor myocarditis due to his elevated cardiac troponin and coronary angiogram with non-obstructive disease, and he was empirically treated with systemic steroids. He also received oral diuretics for presumed new-onset heart failure with preserved ejection fraction.
During this admission, a paracentesis revealed chylous ascites with triglycerides >5000 mg/dL and thoracentesis showed chylothorax. Cytology was negative for malignancy. A computed tomographic (CT) scan showed a 3.2 cm x 2.7 cm paraesophageal lymphocele. Despite treatment with diuretics, a low-fat diet, and paracentesis, his chylous fluid reaccumulated. A multidisciplinary team attempted thoracic duct embolization but were unsuccessful. The patient continues to receive serial therapeutic paracenteses and thoracenteses.
Discussion: Clinicians should maintain a broad differential when evaluating patients with new ascites. Guidelines recommend diagnostic paracentesis in all patients with clinically evident new ascites. Chylous ascites is defined by triglyceride levels >200 mg/dL. It most commonly occurs in lymphatic anomalies or malignancy but can also be caused by cirrhosis, infection, and other less common etiologies. CT scans are helpful to determine the underlying etiology in patients with malignancy or recent surgeries. Lymphoscintigraphy and lymphangiography can assess for lymphatic obstruction or leakage and are considered the gold standard. Treatment is multifarious and relies on dietary adjustments, pharmacologic therapies, and more invasive interventions depending on the etiology. We hypothesize our patient’s lymph node biopsy led to lymphocele formation and resulting lymphatic obstruction. This case emphasizes the importance of paracentesis in evaluating new ascites and the often challenging nature of managing chylous fluid collections.

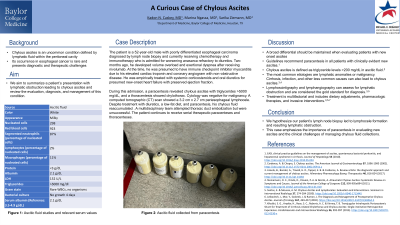
Figure: Figure 1: Peritoneal fluid collected from paracentesis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kadon Caskey indicated no relevant financial relationships.
Marina Ngassa indicated no relevant financial relationships.
Sarika Ziemann indicated no relevant financial relationships.
Kadon Caskey, MD1, Marina Ngassa, MD1, Sarika Ziemann, MD2. P1279 - A Curious Case of Chylous Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
