Sunday Poster Session
Category: Liver
P1292 - A Rare Case of Acute Promyelocytic Leukemia Following Simultaneous Liver-Kidney Transplantation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NO
Nazli Begum Ozturk, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD1, Artem Dadamyan, MS2, Rama Mouhaffel, MD3, Laith H. Jamil, MD2
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Oakland University William Beaumont School of Medicine, Royal Oak, MI; 3Banner - University of Arizona, Tucson, AZ
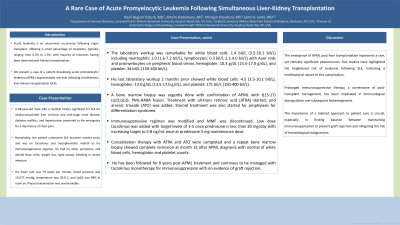
Introduction: Acute leukemia is an uncommon occurrence following organ transplant, effecting a small percentage of recipients, typically ranging from 0.2% to 2.5%. We present a case of a patient developing acute promyelocytic leukemia (APML) approximately one year following simultaneous liver-kidney transplantation (SLK).
Case Description/Methods: A 68-year-old male with a medical history significant for SLK for alcohol-associated liver cirrhosis and end-stage renal disease, and diabetes mellitus presented to the emergency for 2-day history of chest pain. Remarkably, the patient underwent SLK fourteen months prior, and was on tacrolimus and mycophenolate mofetil (MMF). He had no other symptoms, and denied fever, chills, weight loss, night sweats, or bleeding. His heart rate was 79 bpm, blood pressure was 151/75 mmHg, temperature was 36.8 C, and SpO2 was 98% at room air. Physical examination was unremarkable. The laboratory workup showed white blood cells: 1.4 bil/L (3.5-10.1 bil/L) including neutrophils: 1.0 (1.6-7.2 bil/L) and lymphocytes: 0.3 bil/L 1.1-4.0 bil/L) with Auer rods and promyelocytes on peripheral blood smear, hemoglobin: 10.3 g/dL (13.5-17.0 g/dL), and platelet: 34 bil/L (150-400 bil/L). His last laboratory workup 2 months prior showed white blood cells: 4.5 (3.5-10.1 bil/L), hemoglobin: 13.0 g/dL (13.5-17.0 g/dL), and platelet: 171 bil/L (150-400 bil/L). A bone marrow biopsy confirmed APML with t(15:17) (q22;q12); PML-RARA fusion. Treatment with all-trans retinoic acid (ATRA) and arsenic trioxide (ATO) was started, and steroid treatment was added for prophylaxis of differentiation syndrome. Immunosuppressive regimen was modified with MMF discontinuation. Low dose tacrolimus was added with target levels of 3-5 ng/mL once prednisone was < 20 mg/day with increased target to 5-8 ng/mL once prednisone 5 mg/day. Consolidation therapy with ATRA and ATO were completed and a repeat bone marrow biopsy showed complete remission at month 13 after APML diagnosis. He has been followed for 8 years post-APML treatment and continues to be managed with tacrolimus monotherapy for immunosuppression with no evidence of graft rejection.
Discussion: The emergence of APML post-liver transplantation represents a rare, yet clinically significant phenomenon. Prolonged immunosuppressive therapy has been implicated in immunological dysregulation and subsequent leukemogenesis. Tailored approach between maintaining immunosuppression to prevent graft rejection and mitigating the risk of hematological malignancies is crucial.
Disclosures:
Nazli Begum Ozturk, MD1, Artem Dadamyan, MS2, Rama Mouhaffel, MD3, Laith H. Jamil, MD2. P1292 - A Rare Case of Acute Promyelocytic Leukemia Following Simultaneous Liver-Kidney Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Oakland University William Beaumont School of Medicine, Royal Oak, MI; 3Banner - University of Arizona, Tucson, AZ
Introduction: Acute leukemia is an uncommon occurrence following organ transplant, effecting a small percentage of recipients, typically ranging from 0.2% to 2.5%. We present a case of a patient developing acute promyelocytic leukemia (APML) approximately one year following simultaneous liver-kidney transplantation (SLK).
Case Description/Methods: A 68-year-old male with a medical history significant for SLK for alcohol-associated liver cirrhosis and end-stage renal disease, and diabetes mellitus presented to the emergency for 2-day history of chest pain. Remarkably, the patient underwent SLK fourteen months prior, and was on tacrolimus and mycophenolate mofetil (MMF). He had no other symptoms, and denied fever, chills, weight loss, night sweats, or bleeding. His heart rate was 79 bpm, blood pressure was 151/75 mmHg, temperature was 36.8 C, and SpO2 was 98% at room air. Physical examination was unremarkable. The laboratory workup showed white blood cells: 1.4 bil/L (3.5-10.1 bil/L) including neutrophils: 1.0 (1.6-7.2 bil/L) and lymphocytes: 0.3 bil/L 1.1-4.0 bil/L) with Auer rods and promyelocytes on peripheral blood smear, hemoglobin: 10.3 g/dL (13.5-17.0 g/dL), and platelet: 34 bil/L (150-400 bil/L). His last laboratory workup 2 months prior showed white blood cells: 4.5 (3.5-10.1 bil/L), hemoglobin: 13.0 g/dL (13.5-17.0 g/dL), and platelet: 171 bil/L (150-400 bil/L). A bone marrow biopsy confirmed APML with t(15:17) (q22;q12); PML-RARA fusion. Treatment with all-trans retinoic acid (ATRA) and arsenic trioxide (ATO) was started, and steroid treatment was added for prophylaxis of differentiation syndrome. Immunosuppressive regimen was modified with MMF discontinuation. Low dose tacrolimus was added with target levels of 3-5 ng/mL once prednisone was < 20 mg/day with increased target to 5-8 ng/mL once prednisone 5 mg/day. Consolidation therapy with ATRA and ATO were completed and a repeat bone marrow biopsy showed complete remission at month 13 after APML diagnosis. He has been followed for 8 years post-APML treatment and continues to be managed with tacrolimus monotherapy for immunosuppression with no evidence of graft rejection.
Discussion: The emergence of APML post-liver transplantation represents a rare, yet clinically significant phenomenon. Prolonged immunosuppressive therapy has been implicated in immunological dysregulation and subsequent leukemogenesis. Tailored approach between maintaining immunosuppression to prevent graft rejection and mitigating the risk of hematological malignancies is crucial.
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Artem Dadamyan indicated no relevant financial relationships.
Rama Mouhaffel indicated no relevant financial relationships.
Laith Jamil indicated no relevant financial relationships.
Nazli Begum Ozturk, MD1, Artem Dadamyan, MS2, Rama Mouhaffel, MD3, Laith H. Jamil, MD2. P1292 - A Rare Case of Acute Promyelocytic Leukemia Following Simultaneous Liver-Kidney Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
