Sunday Poster Session
Category: Liver
P1195 - Outcomes of Sepsis in Liver Transplant Recipients: Insights From the National Inpatient Sample Database
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HU
Hameed Ullah, MD
Saint Luke's Hospital
St. Louis, MO
Presenting Author(s)
Hameed Ullah, MD1, Muhammad Jahanzaib Khan, MD2, Osama Sherjeel Khan, MD3, Effa Zahid, MD3, Shaheryar Usman, MD4, Elie chahla, MD5, Asad Ur Rahman, MD3
1Saint Luke's Hospital, St. Louis, MO; 2Mather Hospital, Northwell Health, New York, NY; 3Cleveland Clinic Florida, Weston, FL; 4Mather Hospital, Northwell Health, Port Jefferson, NY; 5St. Luke's Hospital, St. Louis, MO
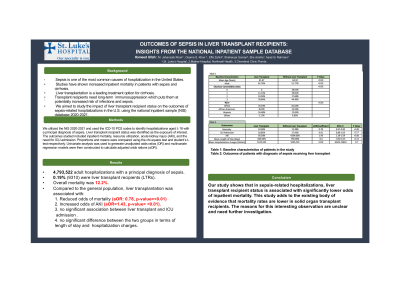
Introduction: Sepsis is one of the most common causes of hospitalization in the United States. Studies have shown increased inpatient mortality in patients with sepsis and cirrhosis. Liver transplantation is a leading treatment option for cirrhosis. Transplant recipients need long-term immunosuppression which puts them at potentially increased risk of infections and sepsis. We aimed to study the impact of liver transplant recipient status on the outcomes of sepsis-related hospitalizations in the U.S. using the national inpatient sample (NIS) database 2020-2021.
Methods: We utilized the NIS 2020-2021 and used the ICD-10 PCS codes to identify hospitalizations aged ≥ 18 with a principal diagnosis of sepsis. Liver transplant recipient status was identified as the exposure of interest. The outcomes studied included inpatient mortality, resource utilization, acute kidney injury (AKI), and the need for ICU admission. Proportions and means were compared using the chi-square test and student’s t-test respectively. Univariate analysis was used to generate unadjusted odds ratios (OR) and multivariate regression models were then constructed to calculate adjusted odds rations (aOR).
Results: Out of 4,793,522 adult hospitalizations with a principal diagnosis of sepsis, 0.19% (9310) were liver transplant recipients (LTRs). The mean age of LTRs was significantly lower (61.67 vs 64.32, p-value= 0.00). Of the LTRs, 61% were males, 70% Caucasians, 8% African Americans, and 16% Hispanics. The overall mortality was 12.2%. On multivariate logistic regression analysis, compared to general population, liver transplantation was associated with significantly reduced odds of mortality (aOR: 0.78, p-value=0.001) and increased odds of AKI (aOR=1.43, p-value= 0.00). There was no significant association between liver transplantation and the need for ICU admission (aOR=0.91, p-value= 0.169). On multivariate linear regression analysis, there was no significant difference between the two groups in terms of length of stay (difference= 0.4 days, p-value= 0.136) and total hospitalization charges (added 2110$, p-value=0.695).
Discussion: Our study shows that in sepsis-related hospitalizations, liver transplant recipient status is associated with significantly lower odds of inpatient mortality. This study adds to the existing body of evidence that mortality rates are lower in solid organ transplant recipients. The reasons for this interesting observation are unclear and need further investigation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hameed Ullah, MD1, Muhammad Jahanzaib Khan, MD2, Osama Sherjeel Khan, MD3, Effa Zahid, MD3, Shaheryar Usman, MD4, Elie chahla, MD5, Asad Ur Rahman, MD3. P1195 - Outcomes of Sepsis in Liver Transplant Recipients: Insights From the National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Luke's Hospital, St. Louis, MO; 2Mather Hospital, Northwell Health, New York, NY; 3Cleveland Clinic Florida, Weston, FL; 4Mather Hospital, Northwell Health, Port Jefferson, NY; 5St. Luke's Hospital, St. Louis, MO
Introduction: Sepsis is one of the most common causes of hospitalization in the United States. Studies have shown increased inpatient mortality in patients with sepsis and cirrhosis. Liver transplantation is a leading treatment option for cirrhosis. Transplant recipients need long-term immunosuppression which puts them at potentially increased risk of infections and sepsis. We aimed to study the impact of liver transplant recipient status on the outcomes of sepsis-related hospitalizations in the U.S. using the national inpatient sample (NIS) database 2020-2021.
Methods: We utilized the NIS 2020-2021 and used the ICD-10 PCS codes to identify hospitalizations aged ≥ 18 with a principal diagnosis of sepsis. Liver transplant recipient status was identified as the exposure of interest. The outcomes studied included inpatient mortality, resource utilization, acute kidney injury (AKI), and the need for ICU admission. Proportions and means were compared using the chi-square test and student’s t-test respectively. Univariate analysis was used to generate unadjusted odds ratios (OR) and multivariate regression models were then constructed to calculate adjusted odds rations (aOR).
Results: Out of 4,793,522 adult hospitalizations with a principal diagnosis of sepsis, 0.19% (9310) were liver transplant recipients (LTRs). The mean age of LTRs was significantly lower (61.67 vs 64.32, p-value= 0.00). Of the LTRs, 61% were males, 70% Caucasians, 8% African Americans, and 16% Hispanics. The overall mortality was 12.2%. On multivariate logistic regression analysis, compared to general population, liver transplantation was associated with significantly reduced odds of mortality (aOR: 0.78, p-value=0.001) and increased odds of AKI (aOR=1.43, p-value= 0.00). There was no significant association between liver transplantation and the need for ICU admission (aOR=0.91, p-value= 0.169). On multivariate linear regression analysis, there was no significant difference between the two groups in terms of length of stay (difference= 0.4 days, p-value= 0.136) and total hospitalization charges (added 2110$, p-value=0.695).
Discussion: Our study shows that in sepsis-related hospitalizations, liver transplant recipient status is associated with significantly lower odds of inpatient mortality. This study adds to the existing body of evidence that mortality rates are lower in solid organ transplant recipients. The reasons for this interesting observation are unclear and need further investigation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Osama Sherjeel Khan indicated no relevant financial relationships.
Effa Zahid indicated no relevant financial relationships.
Shaheryar Usman indicated no relevant financial relationships.
Elie chahla indicated no relevant financial relationships.
Asad Ur Rahman indicated no relevant financial relationships.
Hameed Ullah, MD1, Muhammad Jahanzaib Khan, MD2, Osama Sherjeel Khan, MD3, Effa Zahid, MD3, Shaheryar Usman, MD4, Elie chahla, MD5, Asad Ur Rahman, MD3. P1195 - Outcomes of Sepsis in Liver Transplant Recipients: Insights From the National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
