Sunday Poster Session
Category: Liver
P1203 - Impact of Metabolic and Obesity Phenotypes on Outcomes in Patients With MASLD: Insights From National Inpatient Sample
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Sahiljot Bhupal, MBBS
Dayanand Medical College and Hospital
Chicago, IL
Presenting Author(s)
Sahiljot Bhupal, MBBS1, Anmol Singh, MBBS2, Ramandeep Sandhu, MBBS3, Vikash Kumar, MD4, Aalam Sohal, MD5
1Dayanand Medical College and Hospital, Chicago, IL; 2Tristar Centennial Medical Center, Nashville, TN; 3Creighton University School of Medicine, Phoenix, AZ; 4Creighton University School of Medicine, Brooklyn, NY; 5Creighton University School of Medicine, Seattle, WA
Introduction: Research suggests that the presence of various metabolic risk factors influences the severity and clinical outcomes among patients with MASLD. This has been attributed to genetics and metabolic risk factors in the population. This study aims to analyze the impact of obesity and metabolic risk factors on hepatic and cardiovascular adverse events using national hospitalization data.
Methods: We queried the National Inpatient Sample 2016-2020 to identify adult patients( >18 yrs) with MASLD. Patients with missing demographics, BMI< 20, or mortality were excluded. Data was collected on patient demographics, hospital characteristics, and comorbidities. Patients were stratified into two groups based on the presence of obesity and further stratified into metabolic healthy or unhealthy based on the presence of two or more metabolic risk factors (including diabetes, hypertriglyceridemia, and hypertension). The outcomes studied were liver-related adverse events, cardiovascular events, and chronic kidney disease. The relationship between MASLD phenotypes and outcomes was assessed using the multivariate regression model.
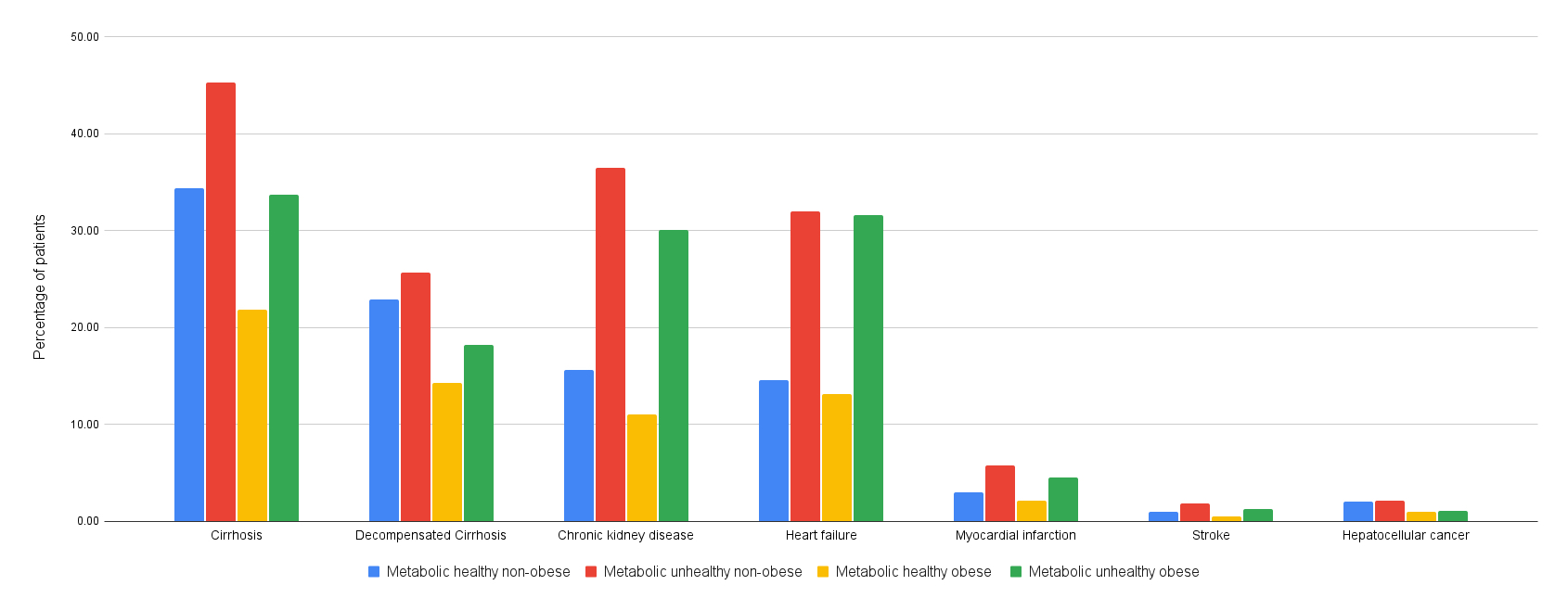
Results: A total of 738,915 patients were included in the analysis. These included 4 groups- metabolic healthy non-obese (30.8%), metabolic unhealthy non-obese (32.8), metabolic healthy obese (15%), and metabolic unhealthy non-obese (21.4%). Metabolically unhealthy non-obese (MUNO) patients had the highest prevalence of cirrhosis (45.3%), myocardial infarction (5.8%), stroke (1.8%), chronic kidney disease (CKD)(36.5%), heart failure (32%) and decompensated cirrhosis (25.7%). The lowest prevalence of these outcomes was noted in metabolically healthy obese (MHO) patients. After adjusting for confounding factors, MUNO had statistically significantly higher odds of cirrhosis ( aOR = 1.69, p< 0.001), myocardial infarction ( aOR = 1.31, p< 0.001), stroke ( aOR = 2.76, p< 0.001), and CKD ( aOR = 2.84, p< 0.001) compared to MHO patients. The highest risk of heart failure was noted in metabolically unhealthy obese patients, compared to MHO (aOR-2.05, p< 0.001).
Discussion: Our study notes that MUNO patients were at a higher risk of not only liver-related adverse events but also cardiovascular events and chronic kidney disease compared to MHO patients. This study suggests that metabolic risk factors play a more important role in influencing the progression of the disease, and modification of these risk factors will be beneficial in improving outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sahiljot Bhupal, MBBS1, Anmol Singh, MBBS2, Ramandeep Sandhu, MBBS3, Vikash Kumar, MD4, Aalam Sohal, MD5. P1203 - Impact of Metabolic and Obesity Phenotypes on Outcomes in Patients With MASLD: Insights From National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Dayanand Medical College and Hospital, Chicago, IL; 2Tristar Centennial Medical Center, Nashville, TN; 3Creighton University School of Medicine, Phoenix, AZ; 4Creighton University School of Medicine, Brooklyn, NY; 5Creighton University School of Medicine, Seattle, WA
Introduction: Research suggests that the presence of various metabolic risk factors influences the severity and clinical outcomes among patients with MASLD. This has been attributed to genetics and metabolic risk factors in the population. This study aims to analyze the impact of obesity and metabolic risk factors on hepatic and cardiovascular adverse events using national hospitalization data.
Methods: We queried the National Inpatient Sample 2016-2020 to identify adult patients( >18 yrs) with MASLD. Patients with missing demographics, BMI< 20, or mortality were excluded. Data was collected on patient demographics, hospital characteristics, and comorbidities. Patients were stratified into two groups based on the presence of obesity and further stratified into metabolic healthy or unhealthy based on the presence of two or more metabolic risk factors (including diabetes, hypertriglyceridemia, and hypertension). The outcomes studied were liver-related adverse events, cardiovascular events, and chronic kidney disease. The relationship between MASLD phenotypes and outcomes was assessed using the multivariate regression model.
Results: A total of 738,915 patients were included in the analysis. These included 4 groups- metabolic healthy non-obese (30.8%), metabolic unhealthy non-obese (32.8), metabolic healthy obese (15%), and metabolic unhealthy non-obese (21.4%). Metabolically unhealthy non-obese (MUNO) patients had the highest prevalence of cirrhosis (45.3%), myocardial infarction (5.8%), stroke (1.8%), chronic kidney disease (CKD)(36.5%), heart failure (32%) and decompensated cirrhosis (25.7%). The lowest prevalence of these outcomes was noted in metabolically healthy obese (MHO) patients. After adjusting for confounding factors, MUNO had statistically significantly higher odds of cirrhosis ( aOR = 1.69, p< 0.001), myocardial infarction ( aOR = 1.31, p< 0.001), stroke ( aOR = 2.76, p< 0.001), and CKD ( aOR = 2.84, p< 0.001) compared to MHO patients. The highest risk of heart failure was noted in metabolically unhealthy obese patients, compared to MHO (aOR-2.05, p< 0.001).
Discussion: Our study notes that MUNO patients were at a higher risk of not only liver-related adverse events but also cardiovascular events and chronic kidney disease compared to MHO patients. This study suggests that metabolic risk factors play a more important role in influencing the progression of the disease, and modification of these risk factors will be beneficial in improving outcomes.
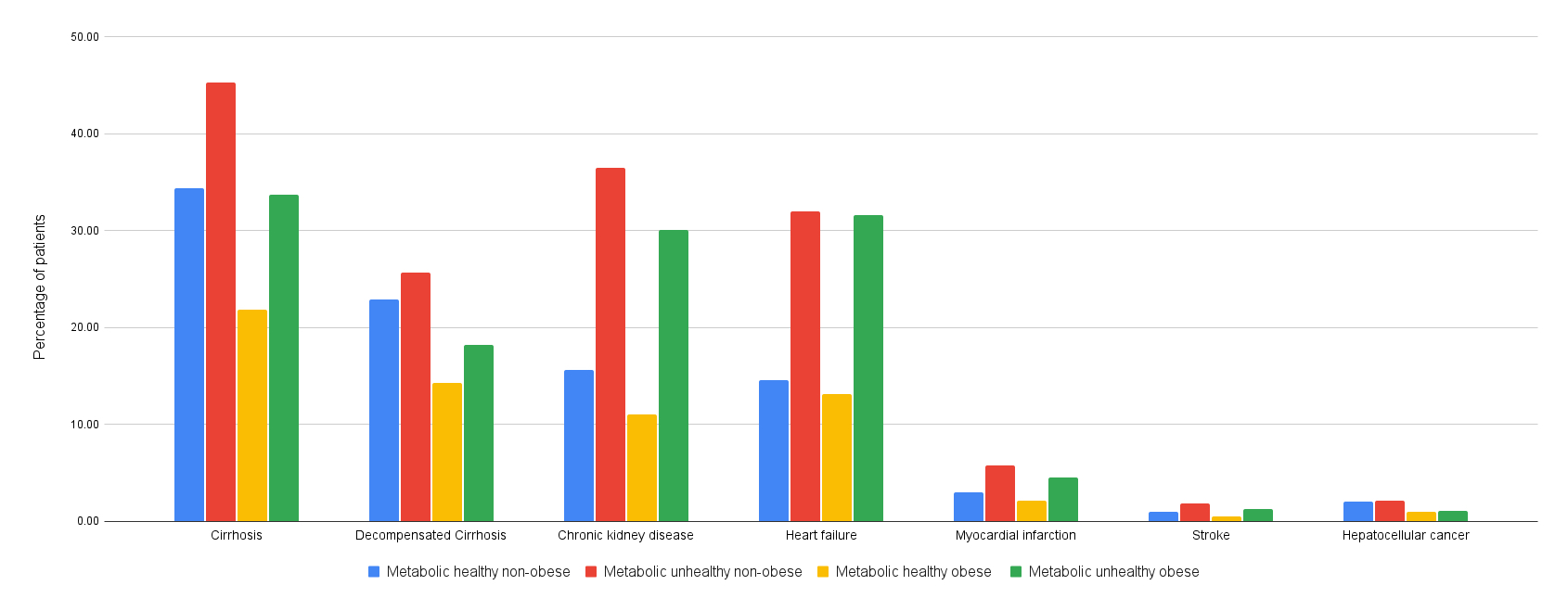
Figure: Figure 1- Outcomes, stratified by the metabolic risk factor and obesity status among patients with MASLD
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sahiljot Bhupal indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Sahiljot Bhupal, MBBS1, Anmol Singh, MBBS2, Ramandeep Sandhu, MBBS3, Vikash Kumar, MD4, Aalam Sohal, MD5. P1203 - Impact of Metabolic and Obesity Phenotypes on Outcomes in Patients With MASLD: Insights From National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
