Sunday Poster Session
Category: Liver
P1208 - Limited Success of Point-of-Care Screening for Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) Related Fibrosis Using FIB-4/Transient Elastography in a Weight Management/Diabetes Clinic
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- CT
Clare Townsend, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Clare Townsend, MD1, Ivania Rizo, MD2, Kathryn Fantasia, MD, MSc2, Arpan Mohanty, MD3
1Boston Medical Center, Boston, MA; 2Boston University Chobanian & Avedisian School of Medicine, Boston, MA; 3Boston University, Boston, MA
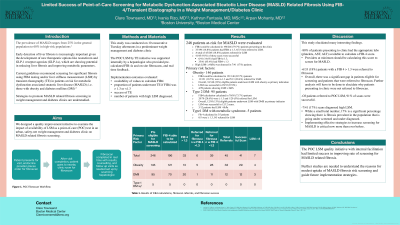
Introduction: Current guidelines recommend screening for significant fibrosis using FIB4 testing and/or liver stiffness measurement (LSM) by transient elastography (TE) in patients at risk for metabolic dysfunction associated steatotic liver disease (MASLD); i.e. those with obesity and diabetes mellitus (DM). Strategies to promote MASLD related fibrosis screening are understudied. We designed a quality improvement initiative to examine the impact of availability of LSM as a point-of-care (POC) test in an urban, safety-net weight management and diabetes clinic on MASLD related fibrosis screening.
Methods: This study was conducted on 10 consecutive Tuesday afternoons in a predominant weight management and diabetes clinic. The POC LSM by TE initiative was supported by a hepatologist who provided pre-calculated FIB-4s and on-site information. The implementation outcomes evaluated were availability of values to calculate FIB4, proportion of patients underwent TE if FIB4 was ≥ 1.3 or < 1.3, success of TE and number of patients with high LSM diagnosed.
Results: 246 patients at-risk for MASLD were evaluated in clinic. Primary risk factors were obesity (146 patients), type 2 DM (95) and type1 DM with metabolic syndrome (5). Among patients with obesity, FIB4 could be calculated in 121/146 (82.7%). Of the available FIB4s, 13/121 (10.7%) were ≥ 1.3 and 5/13 (38.4%) were referred for LSM. Overall, 33 patients underwent LSM with obesity as a primary indication (5 with FIB4 ≥ 1.3; 28 with FIB 4 < 1.3). LSM was successful in 29/33 (87.9%) with 4/29 patients showing LSM > 8kPa. Among patients with Type 2 DM, FIB4 calculation was possible in 70/95 (73.7%). Of the available FIB4 values, 20/70 (28.6%) were ≥ 1.3 with one POC referral for LSM. 11 patients with type 2 DM and FIB4 < 1.3 underwent LSM. Overall, 3/12 patients had LSM >8kPa. All 5 at-risk patients with type 1 DM had FIB4 < 1.3 and were not referred for LSM. In summary, FIB4 could be calculated for 196/246 (79.7%) patients in clinic. Of 33 (16.8%) patients with FIB4 ≥ 1.3, 6 were referred to LSM. A total of 41/246 (16.7%) patients underwent successful LSM, 6/41 (14.6%) had FIB4 ≥ 1.3, 35/41 had FIB4 < 1.3 (85.4%). High LSM ( >8kPa) was detected in 7/41 (17%) patients.
Discussion: The POC LSM quality initiative with internal facilitation had limited success in improving rate of screening for MASLD related fibrosis. Further studies are needed to understand the reasons for modest uptake of MASLD fibrosis risk screening and guide future implementation strategies.
Disclosures:
Clare Townsend, MD1, Ivania Rizo, MD2, Kathryn Fantasia, MD, MSc2, Arpan Mohanty, MD3. P1208 - Limited Success of Point-of-Care Screening for Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) Related Fibrosis Using FIB-4/Transient Elastography in a Weight Management/Diabetes Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Boston University Chobanian & Avedisian School of Medicine, Boston, MA; 3Boston University, Boston, MA
Introduction: Current guidelines recommend screening for significant fibrosis using FIB4 testing and/or liver stiffness measurement (LSM) by transient elastography (TE) in patients at risk for metabolic dysfunction associated steatotic liver disease (MASLD); i.e. those with obesity and diabetes mellitus (DM). Strategies to promote MASLD related fibrosis screening are understudied. We designed a quality improvement initiative to examine the impact of availability of LSM as a point-of-care (POC) test in an urban, safety-net weight management and diabetes clinic on MASLD related fibrosis screening.
Methods: This study was conducted on 10 consecutive Tuesday afternoons in a predominant weight management and diabetes clinic. The POC LSM by TE initiative was supported by a hepatologist who provided pre-calculated FIB-4s and on-site information. The implementation outcomes evaluated were availability of values to calculate FIB4, proportion of patients underwent TE if FIB4 was ≥ 1.3 or < 1.3, success of TE and number of patients with high LSM diagnosed.
Results: 246 patients at-risk for MASLD were evaluated in clinic. Primary risk factors were obesity (146 patients), type 2 DM (95) and type1 DM with metabolic syndrome (5). Among patients with obesity, FIB4 could be calculated in 121/146 (82.7%). Of the available FIB4s, 13/121 (10.7%) were ≥ 1.3 and 5/13 (38.4%) were referred for LSM. Overall, 33 patients underwent LSM with obesity as a primary indication (5 with FIB4 ≥ 1.3; 28 with FIB 4 < 1.3). LSM was successful in 29/33 (87.9%) with 4/29 patients showing LSM > 8kPa. Among patients with Type 2 DM, FIB4 calculation was possible in 70/95 (73.7%). Of the available FIB4 values, 20/70 (28.6%) were ≥ 1.3 with one POC referral for LSM. 11 patients with type 2 DM and FIB4 < 1.3 underwent LSM. Overall, 3/12 patients had LSM >8kPa. All 5 at-risk patients with type 1 DM had FIB4 < 1.3 and were not referred for LSM. In summary, FIB4 could be calculated for 196/246 (79.7%) patients in clinic. Of 33 (16.8%) patients with FIB4 ≥ 1.3, 6 were referred to LSM. A total of 41/246 (16.7%) patients underwent successful LSM, 6/41 (14.6%) had FIB4 ≥ 1.3, 35/41 had FIB4 < 1.3 (85.4%). High LSM ( >8kPa) was detected in 7/41 (17%) patients.
Discussion: The POC LSM quality initiative with internal facilitation had limited success in improving rate of screening for MASLD related fibrosis. Further studies are needed to understand the reasons for modest uptake of MASLD fibrosis risk screening and guide future implementation strategies.
Disclosures:
Clare Townsend indicated no relevant financial relationships.
Ivania Rizo: NovoNordisk – Consultant.
Kathryn Fantasia: Gilead Sciences – Grant/Research Support.
Arpan Mohanty: Gilead – Grant/Research Support. Novo nordisk – Consultant.
Clare Townsend, MD1, Ivania Rizo, MD2, Kathryn Fantasia, MD, MSc2, Arpan Mohanty, MD3. P1208 - Limited Success of Point-of-Care Screening for Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) Related Fibrosis Using FIB-4/Transient Elastography in a Weight Management/Diabetes Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
