Sunday Poster Session
Category: Liver
P1209 - Advanced Liver Disease Detected by Abdominal Imaging Does Not Lead to Linkage to Care in Hepatology Clinics or Uptake of Hepatocellular Carcinoma Screening in an Urban Center
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmed Ebeid, MD
George Washington University
Arlington, VA
Presenting Author(s)
Ahmed Ebeid, MD1, Abdelrhman Refaey, MD1, Nakul Ganju, BS2, Mrudula Bandaru, MD2, Omar Saadi, BS2, Issa Ali, BS2, Ameer Abutaleb, MD3
1George Washington University, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3George Washington University Hospital, Washington, DC
Introduction: Cirrhosis is the 11th most common cause of death and the third cause in individuals aged 45–64 years. Imaging is increasingly used to diagnose cirrhosis without a liver biopsy. MRI has a sensitivity of 86% and a specificity of 93%, while ultrasound, when examining surface nodularity, has a sensitivity of 91% and a specificity of 94%. Our goal is to evaluate the use of imaging to identify cirrhosis and subsequent hepatocellular carcinoma, and whether patients are linked to a hepatologist for further evaluation.
Methods: We conducted a retrospective chart review of patients with a diagnosis of cirrhosis enrolled in the electronic medical records of the George Washington Hospital and outpatient clinics, from January 1, 2022, to December 31, 2023. We included all subjects aged over 18 years with an ICD-10 diagnosis code of cirrhosis and a source of abdominal imaging. Patients with a history of hepatocellular carcinoma or liver transplant were excluded from the study. We evaluated if those patients showed imaging-based cirrhosis and if they underwent a 6 month- follow up imaging as a standard screening for hepatocellular carcinoma. We conducted a descriptive analysis among patients with the diagnosis code of cirrhosis and an imaging study. Among those patients, we used both ANOVA and Chi Sq / Fisher exact statistical tests.
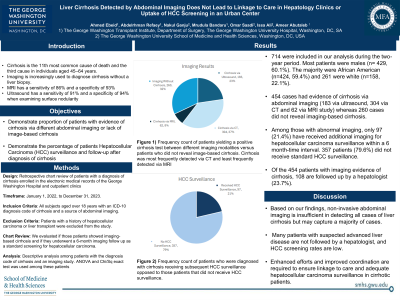
Results: 714 were included in our analysis during the two-year period. Most patients were males (n= 429, 60.1%). The majority were African American (n=424, 59.4%) and 261 were white (n=158, 22.1%). 454 cases had evidence of cirrhosis via abdominal imaging (183 via ultrasound, 304 via CT and 62 via MRI study) whereas 260 cases did not reveal imaging-based cirrhosis. Among those with abnormal imaging, only 97 (21.4%) have received additional imaging for hepatocellular carcinoma surveillance within a 6 month-time interval. 357 patients (79.6%) did not receive standard HCC surveillance. Of the 454 patients with imaging evidence of cirrhosis, 108 are followed up by a hepatologist (23.7 %)
Discussion: Based on our findings, non-invasive abdominal imaging is insufficient in detecting all cases of liver cirrhosis but may capture a majority of cases. Many patients with suspected advanced liver disease are not followed by a hepatologist, and HCC screening rates are low. Enhanced efforts and improved coordination are required to ensure linkage to care and adequate hepatocellular carcinoma surveillance in cirrhotic patients.
Disclosures:
Ahmed Ebeid, MD1, Abdelrhman Refaey, MD1, Nakul Ganju, BS2, Mrudula Bandaru, MD2, Omar Saadi, BS2, Issa Ali, BS2, Ameer Abutaleb, MD3. P1209 - Advanced Liver Disease Detected by Abdominal Imaging Does Not Lead to Linkage to Care in Hepatology Clinics or Uptake of Hepatocellular Carcinoma Screening in an Urban Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1George Washington University, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3George Washington University Hospital, Washington, DC
Introduction: Cirrhosis is the 11th most common cause of death and the third cause in individuals aged 45–64 years. Imaging is increasingly used to diagnose cirrhosis without a liver biopsy. MRI has a sensitivity of 86% and a specificity of 93%, while ultrasound, when examining surface nodularity, has a sensitivity of 91% and a specificity of 94%. Our goal is to evaluate the use of imaging to identify cirrhosis and subsequent hepatocellular carcinoma, and whether patients are linked to a hepatologist for further evaluation.
Methods: We conducted a retrospective chart review of patients with a diagnosis of cirrhosis enrolled in the electronic medical records of the George Washington Hospital and outpatient clinics, from January 1, 2022, to December 31, 2023. We included all subjects aged over 18 years with an ICD-10 diagnosis code of cirrhosis and a source of abdominal imaging. Patients with a history of hepatocellular carcinoma or liver transplant were excluded from the study. We evaluated if those patients showed imaging-based cirrhosis and if they underwent a 6 month- follow up imaging as a standard screening for hepatocellular carcinoma. We conducted a descriptive analysis among patients with the diagnosis code of cirrhosis and an imaging study. Among those patients, we used both ANOVA and Chi Sq / Fisher exact statistical tests.
Results: 714 were included in our analysis during the two-year period. Most patients were males (n= 429, 60.1%). The majority were African American (n=424, 59.4%) and 261 were white (n=158, 22.1%). 454 cases had evidence of cirrhosis via abdominal imaging (183 via ultrasound, 304 via CT and 62 via MRI study) whereas 260 cases did not reveal imaging-based cirrhosis. Among those with abnormal imaging, only 97 (21.4%) have received additional imaging for hepatocellular carcinoma surveillance within a 6 month-time interval. 357 patients (79.6%) did not receive standard HCC surveillance. Of the 454 patients with imaging evidence of cirrhosis, 108 are followed up by a hepatologist (23.7 %)
Discussion: Based on our findings, non-invasive abdominal imaging is insufficient in detecting all cases of liver cirrhosis but may capture a majority of cases. Many patients with suspected advanced liver disease are not followed by a hepatologist, and HCC screening rates are low. Enhanced efforts and improved coordination are required to ensure linkage to care and adequate hepatocellular carcinoma surveillance in cirrhotic patients.
Disclosures:
Ahmed Ebeid indicated no relevant financial relationships.
Abdelrhman Refaey indicated no relevant financial relationships.
Nakul Ganju indicated no relevant financial relationships.
Mrudula Bandaru indicated no relevant financial relationships.
Omar Saadi indicated no relevant financial relationships.
Issa Ali indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Ahmed Ebeid, MD1, Abdelrhman Refaey, MD1, Nakul Ganju, BS2, Mrudula Bandaru, MD2, Omar Saadi, BS2, Issa Ali, BS2, Ameer Abutaleb, MD3. P1209 - Advanced Liver Disease Detected by Abdominal Imaging Does Not Lead to Linkage to Care in Hepatology Clinics or Uptake of Hepatocellular Carcinoma Screening in an Urban Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
