Sunday Poster Session
Category: Liver
P1213 - Lipid Lowering Therapies and Primary Sclerosing Cholangitis: A Mendelian Randomization Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MP
Manish Paranjpe, MD
Stanford Health Care
Stanford, CA
Presenting Author(s)
Award: Presidential Poster Award
Manish Paranjpe, MD
Stanford Health Care, Stanford, CA
Introduction: Observational studies have implicated statin use with decreased risk of developing primary sclerosing cholangitis, among other chronic liver diseases. Residual confounding and reverse causality bias limits the interpretability of these observational studies. Whether there is causal association between lipid-lowering therapies and the development of PSC is unknown. The present study sought to investigate whether LDL-C lowering therapy is causally associated with a decreased risk of PSC. We further investigated whether potential associations are driven by HMG-CoA reductase-independent or HMG-CoA dependent mechanisms.
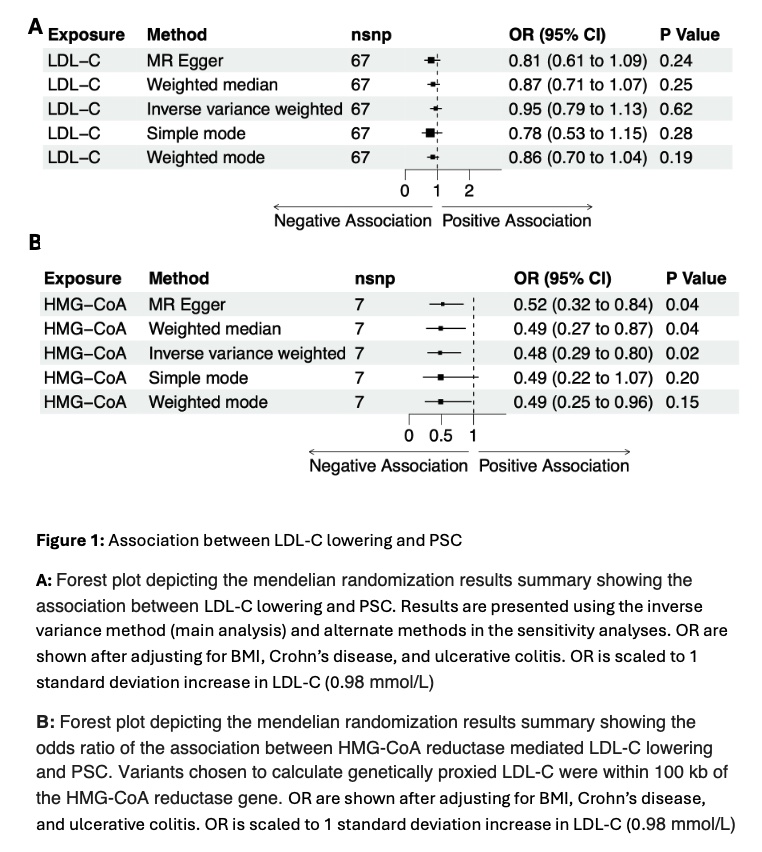
Methods: In the present study, we took a two sample mendelian randomization (MR) approach to understand the causal association between LDL-C lowering and PSC. Genetically proxied LDL-C lowering was determined using summary statistic data from the Global Lipids Genetics Consortium (n=188,577). A total of 67 independent genetic variants (r-squared < 0.001 and located at least 1 Mb apart from each other) were chosen to proxy LDL-C lowering. HMG-CoA dependent analyses were conducted by restricting genetic variants to within 100 kb of the HMC-CoA reductase gene, yielding a total of 7 variants. Genetically proxied risk of primary sclerosing cholangitis was determined using summary statistics from a genome-wide association study of 4,796 PSC cases and 19,955 controls. Mendelian randomization estimates were estimated using the fixed-effect inverse-variance method as the main method. Sensitivity analyses were performed using weighted median, MR-Egger, and MR-PRESSO algorithms. The effect sizes were calculated per 1 standard deviation decrease in plasma LDL-C level (equal to 0.98 mmol/L).
Results: Genetically-predicted LDL-C lowering was not associated with a decreased risk of PSC in the main analysis (OR 0.95, 95% CI: 0.79-1.13, P value 0.62). Interestingly, when restricted to variants within the HMG-CoA reductase gene, a significant effect of LDL-C lowering on PSC was observed (OR 0.48, 95% CI: 0.28-0.8, P value: 0.02). Associations remained consistent after adjusting for genetically predicted smoking status, Crohn’s disease and ulcerative colitis.
Discussion: This mendelian randomization study supports the notion that lipid-lowering therapy is causally associated with a decreased risk of developing PSC. Interestingly, this relationship is only observed in an HMG-CoA dependent LDL-C mechanism. Further mechanistic studies are needed to explore this association.
Disclosures:
Manish Paranjpe, MD. P1213 - Lipid Lowering Therapies and Primary Sclerosing Cholangitis: A Mendelian Randomization Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Manish Paranjpe, MD
Stanford Health Care, Stanford, CA
Introduction: Observational studies have implicated statin use with decreased risk of developing primary sclerosing cholangitis, among other chronic liver diseases. Residual confounding and reverse causality bias limits the interpretability of these observational studies. Whether there is causal association between lipid-lowering therapies and the development of PSC is unknown. The present study sought to investigate whether LDL-C lowering therapy is causally associated with a decreased risk of PSC. We further investigated whether potential associations are driven by HMG-CoA reductase-independent or HMG-CoA dependent mechanisms.
Methods: In the present study, we took a two sample mendelian randomization (MR) approach to understand the causal association between LDL-C lowering and PSC. Genetically proxied LDL-C lowering was determined using summary statistic data from the Global Lipids Genetics Consortium (n=188,577). A total of 67 independent genetic variants (r-squared < 0.001 and located at least 1 Mb apart from each other) were chosen to proxy LDL-C lowering. HMG-CoA dependent analyses were conducted by restricting genetic variants to within 100 kb of the HMC-CoA reductase gene, yielding a total of 7 variants. Genetically proxied risk of primary sclerosing cholangitis was determined using summary statistics from a genome-wide association study of 4,796 PSC cases and 19,955 controls. Mendelian randomization estimates were estimated using the fixed-effect inverse-variance method as the main method. Sensitivity analyses were performed using weighted median, MR-Egger, and MR-PRESSO algorithms. The effect sizes were calculated per 1 standard deviation decrease in plasma LDL-C level (equal to 0.98 mmol/L).
Results: Genetically-predicted LDL-C lowering was not associated with a decreased risk of PSC in the main analysis (OR 0.95, 95% CI: 0.79-1.13, P value 0.62). Interestingly, when restricted to variants within the HMG-CoA reductase gene, a significant effect of LDL-C lowering on PSC was observed (OR 0.48, 95% CI: 0.28-0.8, P value: 0.02). Associations remained consistent after adjusting for genetically predicted smoking status, Crohn’s disease and ulcerative colitis.
Discussion: This mendelian randomization study supports the notion that lipid-lowering therapy is causally associated with a decreased risk of developing PSC. Interestingly, this relationship is only observed in an HMG-CoA dependent LDL-C mechanism. Further mechanistic studies are needed to explore this association.
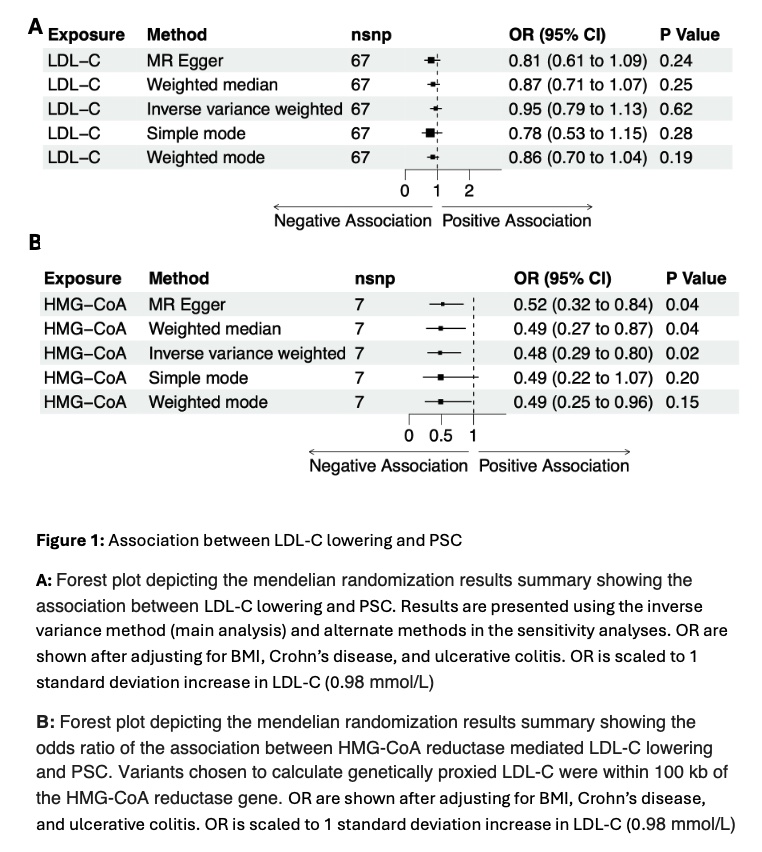
Figure: A: Forest plot depicting the mendelian randomization results summary showing the association between LDL-C lowering and PSC. Results are presented using the inverse variance method (main analysis) and alternate methods in the sensitivity analyses. OR are shown after adjusting for BMI, Crohn’s disease, and ulcerative colitis. OR is scaled to 1 standard deviation increase in LDL-C (0.98 mmol/L)
B: Forest plot depicting the mendelian randomization results summary showing the odds ratio of the association between HMG-CoA reductase mediated LDL-C lowering and PSC. Variants chosen to calculate genetically proxied LDL-C were within 100 kb of the HMG-CoA reductase gene. OR are shown after adjusting for BMI, Crohn’s disease, and ulcerative colitis. OR is scaled to 1 standard deviation increase in LDL-C (0.98 mmol/L)
B: Forest plot depicting the mendelian randomization results summary showing the odds ratio of the association between HMG-CoA reductase mediated LDL-C lowering and PSC. Variants chosen to calculate genetically proxied LDL-C were within 100 kb of the HMG-CoA reductase gene. OR are shown after adjusting for BMI, Crohn’s disease, and ulcerative colitis. OR is scaled to 1 standard deviation increase in LDL-C (0.98 mmol/L)
Disclosures:
Manish Paranjpe indicated no relevant financial relationships.
Manish Paranjpe, MD. P1213 - Lipid Lowering Therapies and Primary Sclerosing Cholangitis: A Mendelian Randomization Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

