Sunday Poster Session
Category: Liver
P1142 - Outcomes in Admissions for Acute Cholangitis in Liver Transplant Recipients: A Nationwide Perspective
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bhanu Siva Mohan Pinnam, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD3, Abdul Mohammed, MD4, Clive J. Miranda, DO, MSc5, Abhin Sapkota, MD1, Chun-Wei Pan, MD1, Sanket Basida, MD6, Sahib Singh, MD7, Hema S. Pinnam, 8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Sumant Inamdar, MD9
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 3The University of Kansas School of Medicine, Kansas City, KS; 4AdventHealth, Orlando, FL; 5CHI Health Creighton University Medical Center, Omaha, NE; 6University of Missouri School of Medicine, Columbia, MO; 7Sinai Hospital, Baltimore, MD; 8Jagadguru Sri Shivarathreeshwara Medical College, Mysuru, Karnataka, India; 9University of Arkansas for Medical Sciences, Little Rock, AR
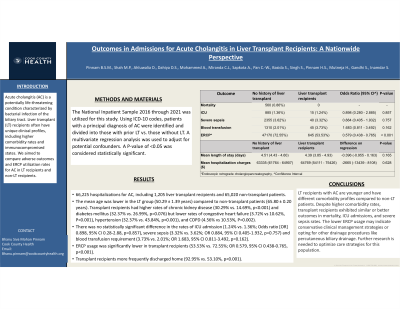
Introduction: Acute cholangitis (AC) is a potentially life-threatening bacterial infection of the biliary tract. Liver transplant (LT) recipients often have unique clinical profiles, including higher comorbidity rates and immunocompromised states. We aimed to compare adverse outcomes and ERCP utilization rates for AC in LT recipients and non-LT recipients.
Methods: The National Inpatient Sample 2016 through 2021 was utilized for this study. Using ICD-10 codes, patients with a principal diagnosis of AC were identified and divided into those with prior LT vs. those without LT. A multivariate regression analysis was used to adjust for potential confounders. A P-value of < 0.05 was considered statistically significant.
Results: A total of 66,225 hospitalizations for AC were identified, including 1,205 liver transplant recipients and 65,020 non-transplant patients. The mean age was lower in the LT group (50.29 ± 1.39 years) compared to non-transplant patients (65.80 ± 0.20 years). Transplant recipients had higher rates of chronic kidney disease (30.29% vs. 14.69%, p< 0.001) and diabetes mellitus (32.37% vs. 26.99%, p=0.076) but lower rates of congestive heart failure (3.72% vs 10.62%, P< 0.001), hypertension (32.37% vs. 43.84%, p< 0.001), and COPD (4.56% vs 10.53%, P=0.002). The mortality rate was 0.86% in non-LT patients and 0% among LT recipients. There was no statistically significant difference in the rates of ICU admission (1.24% vs. 1.36%; Odds ratio [OR] 0.898, 95% CI 0.28-2.88, p=0.857), severe sepsis (3.32% vs. 3.62%; OR 0.884, 95% CI 0.405-1.932, p=0.757) and blood transfusion requirement (3.73% vs. 2.01%; OR 1.683, 95% CI 0.811-3.492, p=0.162).
ERCP usage was significantly lower in transplant recipients (53.53% vs. 72.55%; OR 0.579, 95% CI 0.438-0.765, p< 0.001). Discharge disposition differed significantly, with transplant recipients more frequently discharged home (92.95% vs. 53.10%, p< 0.001). They were also less likely to be transferred to other facilities or require home healthcare.
Discussion: LT recipients with AC are younger and have different comorbidity profiles compared to non-LT patients. Despite higher comorbidity rates, transplant recipients exhibited similar or better outcomes in mortality, ICU admissions, and severe sepsis rates. The lower ERCP usage may indicate conservative clinical management strategies or opting for other drainage procedures like percutaneous biliary drainage. Further research is needed to optimize care strategies for this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD3, Abdul Mohammed, MD4, Clive J. Miranda, DO, MSc5, Abhin Sapkota, MD1, Chun-Wei Pan, MD1, Sanket Basida, MD6, Sahib Singh, MD7, Hema S. Pinnam, 8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Sumant Inamdar, MD9. P1142 - Outcomes in Admissions for Acute Cholangitis in Liver Transplant Recipients: A Nationwide Perspective, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 3The University of Kansas School of Medicine, Kansas City, KS; 4AdventHealth, Orlando, FL; 5CHI Health Creighton University Medical Center, Omaha, NE; 6University of Missouri School of Medicine, Columbia, MO; 7Sinai Hospital, Baltimore, MD; 8Jagadguru Sri Shivarathreeshwara Medical College, Mysuru, Karnataka, India; 9University of Arkansas for Medical Sciences, Little Rock, AR
Introduction: Acute cholangitis (AC) is a potentially life-threatening bacterial infection of the biliary tract. Liver transplant (LT) recipients often have unique clinical profiles, including higher comorbidity rates and immunocompromised states. We aimed to compare adverse outcomes and ERCP utilization rates for AC in LT recipients and non-LT recipients.
Methods: The National Inpatient Sample 2016 through 2021 was utilized for this study. Using ICD-10 codes, patients with a principal diagnosis of AC were identified and divided into those with prior LT vs. those without LT. A multivariate regression analysis was used to adjust for potential confounders. A P-value of < 0.05 was considered statistically significant.
Results: A total of 66,225 hospitalizations for AC were identified, including 1,205 liver transplant recipients and 65,020 non-transplant patients. The mean age was lower in the LT group (50.29 ± 1.39 years) compared to non-transplant patients (65.80 ± 0.20 years). Transplant recipients had higher rates of chronic kidney disease (30.29% vs. 14.69%, p< 0.001) and diabetes mellitus (32.37% vs. 26.99%, p=0.076) but lower rates of congestive heart failure (3.72% vs 10.62%, P< 0.001), hypertension (32.37% vs. 43.84%, p< 0.001), and COPD (4.56% vs 10.53%, P=0.002). The mortality rate was 0.86% in non-LT patients and 0% among LT recipients. There was no statistically significant difference in the rates of ICU admission (1.24% vs. 1.36%; Odds ratio [OR] 0.898, 95% CI 0.28-2.88, p=0.857), severe sepsis (3.32% vs. 3.62%; OR 0.884, 95% CI 0.405-1.932, p=0.757) and blood transfusion requirement (3.73% vs. 2.01%; OR 1.683, 95% CI 0.811-3.492, p=0.162).
ERCP usage was significantly lower in transplant recipients (53.53% vs. 72.55%; OR 0.579, 95% CI 0.438-0.765, p< 0.001). Discharge disposition differed significantly, with transplant recipients more frequently discharged home (92.95% vs. 53.10%, p< 0.001). They were also less likely to be transferred to other facilities or require home healthcare.
Discussion: LT recipients with AC are younger and have different comorbidity profiles compared to non-LT patients. Despite higher comorbidity rates, transplant recipients exhibited similar or better outcomes in mortality, ICU admissions, and severe sepsis rates. The lower ERCP usage may indicate conservative clinical management strategies or opting for other drainage procedures like percutaneous biliary drainage. Further research is needed to optimize care strategies for this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Mihir Shah indicated no relevant financial relationships.
Daksh Ahluwalia indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Sahib Singh indicated no relevant financial relationships.
Hema Pinnam indicated no relevant financial relationships.
Hemant Mutneja indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Sumant Inamdar indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD3, Abdul Mohammed, MD4, Clive J. Miranda, DO, MSc5, Abhin Sapkota, MD1, Chun-Wei Pan, MD1, Sanket Basida, MD6, Sahib Singh, MD7, Hema S. Pinnam, 8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Sumant Inamdar, MD9. P1142 - Outcomes in Admissions for Acute Cholangitis in Liver Transplant Recipients: A Nationwide Perspective, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
